How is Chronic Venous Insufficiency treated?
LJVascular2024-07-06T06:51:16-07:00Unlocking Wellness: Navigating Chronic Venous Insufficiency with Expert Guidance
Chronic Venous Insufficiency (CVI) emerges from untreated venous reflux disease, culminating in an array of uncomfortable symptoms and potential skin complications. In this article, we’ll explore the nuances of CVI, unraveling its symptoms and treatments to guide you through this medical condition.
Deciphering Chronic Venous Insufficiency (CVI)
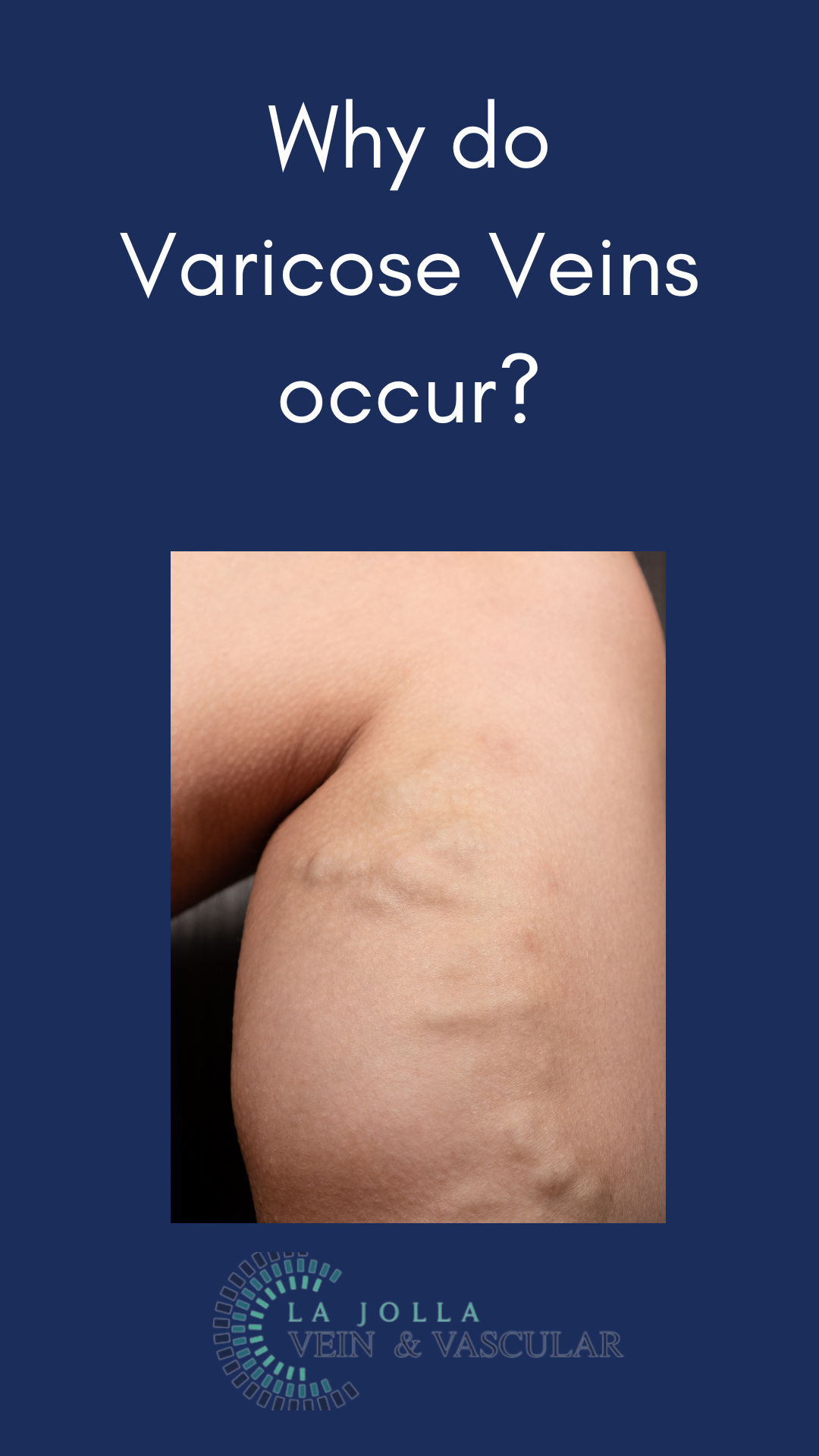
CVI, a chronic inflammatory condition stemming from prolonged venous reflux disease, manifests through distressing symptoms like leg swelling, heaviness, fatigue, and the emergence of varicose veins. However, as CVI progresses, it impairs blood circulation in the leg veins, triggering visible skin alterations termed venous stasis. These skin changes present as darkening, dryness, itching, and firmness around the ankles. In severe instances, skin deterioration leads to ulceration, known as stasis or venous ulcers.
Skin Transformations in CVI
Several skin changes accompany venous insufficiency, including:
- Darkening of the skin along the ankles
- Itching and dry skin around the ankles (venous eczema)
- Formation of wounds around the ankles (venous leg ulcers)
- Understanding CVI Treatment
Although treatment cannot reverse existing skin changes in CVI, it can forestall further degradation and ulceration. Addressing the underlying venous reflux diminishes inflammatory changes, potentially alleviating itchiness and dryness. Yet, persistent skin discoloration might endure despite successful reflux treatment. Central to treatment is rectifying the underlying venous reflux.
Managing Venous Leg Ulcers
Venous leg ulcers, a potential outcome of severe CVI, demand a comprehensive healing approach. Treatments may involve:
- Rectifying the underlying venous reflux
- Referral to a specialized wound care clinic
- Implementing compression therapy
A comprehensive ultrasound examination determines the precise location of the underlying reflux, whether in the saphenous veins, perforator veins, tributaries, or deep veins, guiding the appropriate treatment trajectory.
Chronic Venous Insufficiency entails complex implications for those affected. Armed with understanding the condition, its symptoms, and available treatments, individuals can make informed health decisions, navigating the path to wellness.
Seeking Chronic Venous Insufficiency Treatment in San Diego? Contact La Jolla Vein & Vascular, the best vein clinic in San Diego.
“Bringing Experts Together for Unparalleled Vein and Vascular Care”
La Jolla Vein & Vascular (formerly La Jolla Vein Care) is committed to bringing experts together for unparalleled vein and vascular care.
Nisha Bunke, MD, Sarah Lucas, MD, and Amanda Steinberger, MD are specialists who combine their experience and expertise to offer world-class vascular care.
Our accredited center is also a nationally known teaching site and center of excellence.
For more information on treatments and to book a consultation, please give our office a call at 858-550-0330.
For a deeper dive into vein and vascular care, please check out our Youtube Channel at this link, and our website https://ljvascular.com
For more information on varicose veins and eliminating underlying venous insufficiency,
Please follow our social media Instagram Profile for more fun videos and educational information.
For more blogs and educational content, please check out our clinic’s blog posts!