A patient’s guide to Radiofrequency perforator ablation procedure
LJVascular2024-05-13T23:29:31-07:00Radiofrequency perforator ablation emerges as a crucial procedure for addressing perforator veins, the short connections between deep and superficial veins. These veins, vital for maintaining proper circulation, can suffer from valve damage and retrograde blood flow, leading to various vein disorders and potential skin complications. Understanding the function of perforator veins and the treatment process for their dysfunction is paramount for individuals seeking relief from associated symptoms.
What are Perforator Veins?
Patient’s Guide to Radiofrequency Perforator Ablation
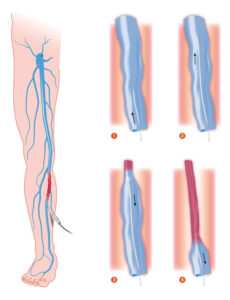
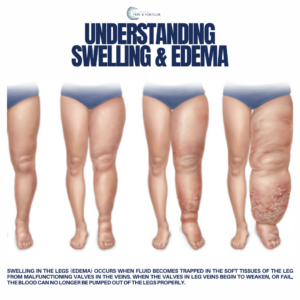
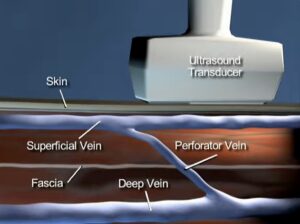
Perforator veins act as bridges between the superficial and deep venous systems in the extremities, facilitating the flow of blood from superficial veins to deep veins. Equipped with one-way valves, these veins prevent the backflow of blood and maintain efficient circulation. However, when these valves malfunction, reflux occurs, leading to an accumulation of blood and pressure, causing incompetence in both superficial veins and perforator veins. This dysfunction, particularly prevalent in the lower leg and ankle, can result in edema, skin discoloration, dermatitis, and even skin ulcers.
Indications for Treatment
Individuals experiencing venous leg ulcers, pre-ulcerative skin changes, persistent varicose veins, leg pain, or swelling may benefit from radiofrequency perforator ablation. By addressing the underlying cause of these symptoms, this outpatient procedure aims to restore proper venous function and alleviate discomfort.
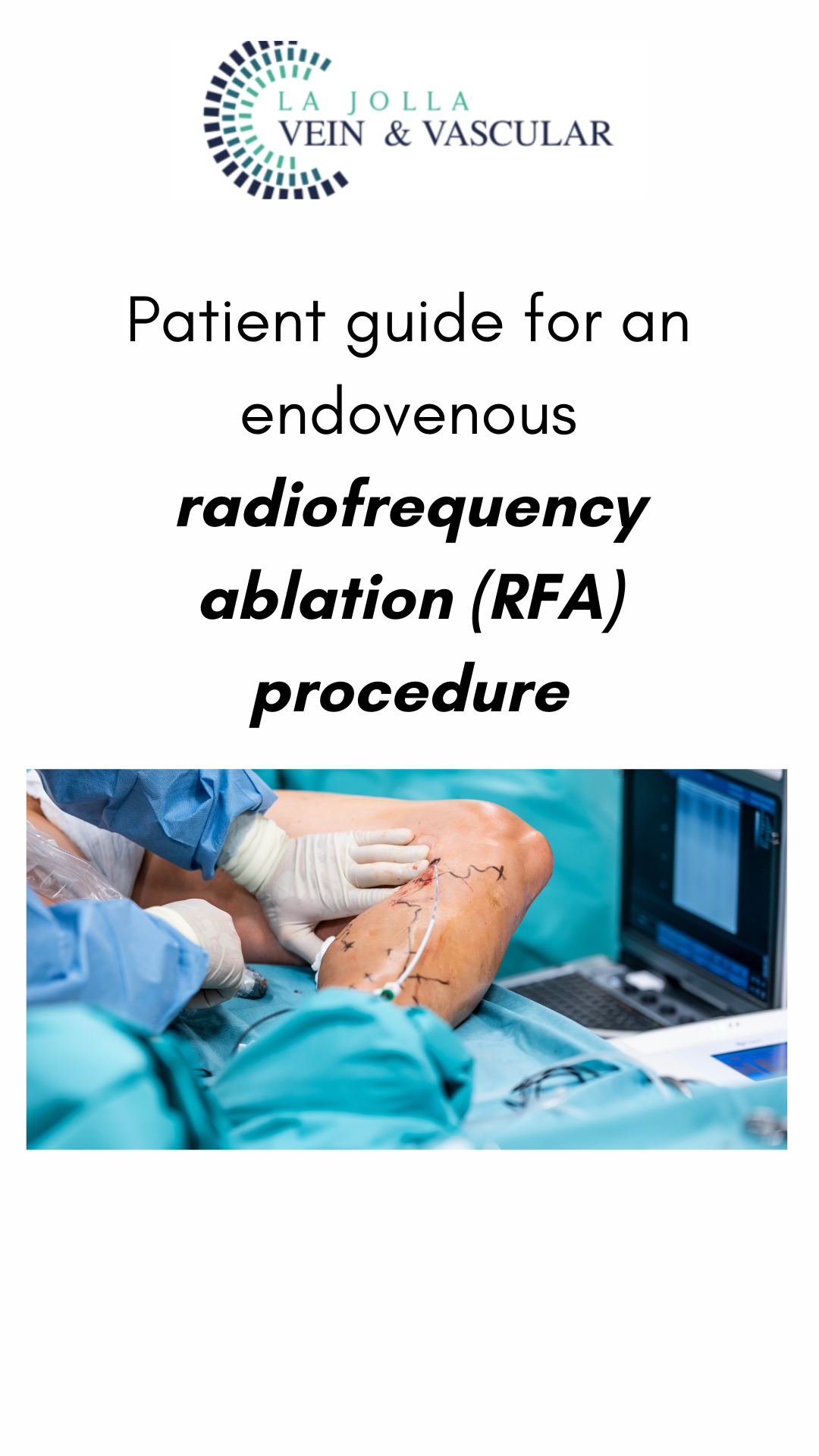
How Does the Treatment Work?
Radiofrequency perforator ablation is a minimally invasive outpatient procedure performed in the doctor’s office. Using ultrasound guidance, a fine needle is inserted into the perforator vein, delivering radiofrequency energy to shrink and eliminate abnormal flow between deep and varicose veins. The procedure typically lasts around 10 minutes per perforator vein, with some patients requiring treatment for multiple veins on the same leg.
What to Expect on the Day of Treatment?
The procedure is performed under local anesthesia, with optional mild oral sedation for patient comfort. Patients are positioned according to the vein being treated and offered amenities like watching a movie or listening to music. After sterile preparation and ultrasound mapping of the veins, a numbing agent is injected, followed by the insertion of the radiofrequency catheter. The vein is then painlessly treated with radiofrequency energy, and a compression stocking is applied for 72 hours post-treatment.
Aftercare and Possible Adverse Effects
Following treatment, patients are advised to walk for 30 minutes twice daily to alleviate discomfort and prevent blood pooling in the legs. Avoidance of strenuous activities, airline travel, saunas, and leg massages for specified periods minimizes the risk of complications. Common side effects include aching in the treated veins and bruising, which typically resolve within a few weeks.
Radiofrequency perforator ablation offers a promising solution for individuals suffering from vein disorders, providing effective symptom relief with minimal downtime. By addressing the underlying cause of venous reflux, this procedure promotes improved circulation and enhances overall vein health, allowing individuals to regain comfort and confidence in their daily lives. If you’re experiencing symptoms of vein disorders, consult with us today to explore the benefits of radiofrequency perforator ablation and take the first step towards healthier veins.
“Bringing Experts Together for Unparalleled Vein and Vascular Care”
La Jolla Vein & Vascular (formerly La Jolla Vein Care) is committed to bringing experts together for unparalleled vein and vascular care.
Nisha Bunke, MD, Sarah Lucas, MD, and Amanda Steinberger, MD are specialists who combine their experience and expertise to offer world-class vascular care.
Our accredited center is also a nationally known teaching site and center of excellence.
For more information on treatments and to book a consultation, please give our office a call at 858-550-0330.
For a deeper dive into vein and vascular care, please check out our Youtube Channel at this link, and our website https://ljvascular.com
For more information on varicose veins and eliminating underlying venous insufficiency,
Please follow our social media Instagram Profile for more fun videos and educational information.
For more blogs and educational content, please check out our clinic’s blog posts!