Sealing wellness: A deep dive into the Venaseal procedure for vascular health
LJVascular2024-10-28T07:23:18-07:00Sealing Wellness: A Deep Dive into the Venaseal Procedure for Vascular Health
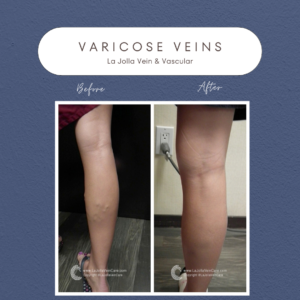
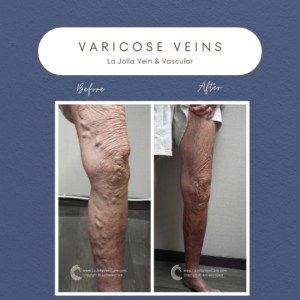
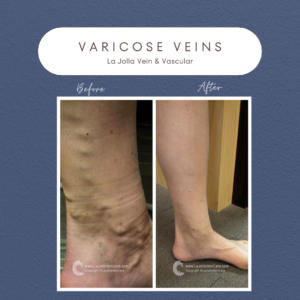
The VenaSeal™ closure system, approved by the U.S. Food and Drug Administration (FDA), offers an innovative and effective way to treat varicose veins. Unlike traditional methods, this minimally invasive procedure utilizes a unique medical adhesive to permanently seal affected superficial veins. In this blog post, we will explore how the VenaSeal system works, its key benefits, and why it stands out as a safe and convenient option for varicose vein treatment.
Understanding the VenaSeal Sapheon Closure System
The VenaSeal Sapheon Closure System represents a revolutionary approach to treating varicose veins, also known as venous reflux disease. Here’s how it works:
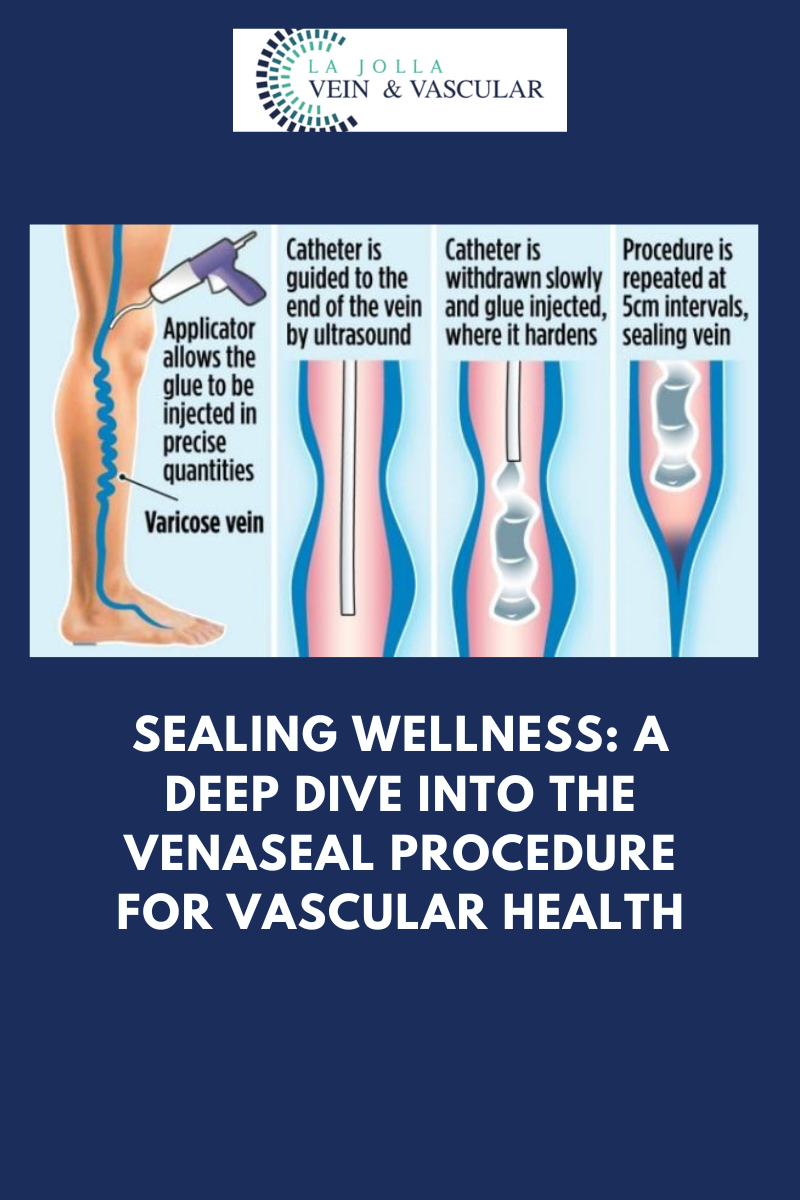
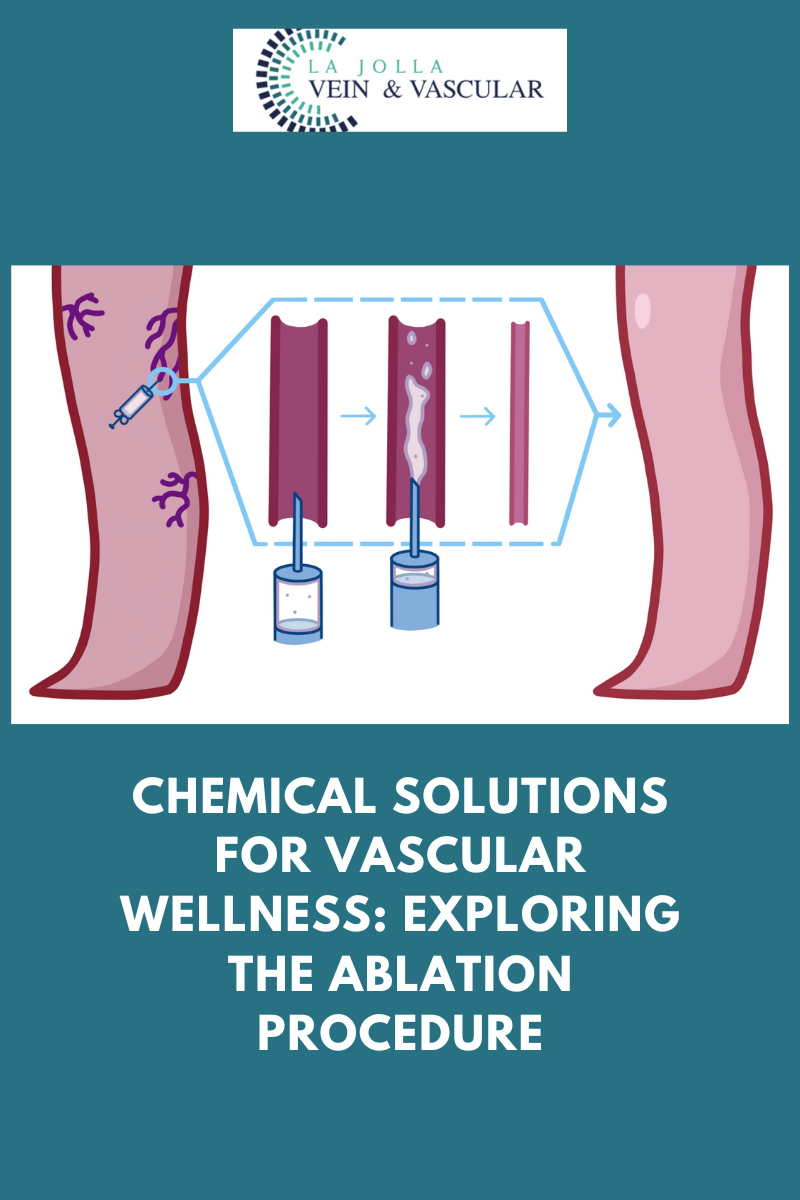
- Minimally Invasive Procedure: The procedure begins with the doctor using ultrasound guidance to navigate a tiny catheter through a small access site in the skin and into the affected vein.
- Medical Glue Application: The VenaSeal™ dispenser then delivers a small amount of medical glue to close the vein. This adhesive effectively seals the problematic vein, preventing further reflux.
- Immediate Blood Rerouting: Once the affected vein is sealed, the body immediately redirects blood flow through other healthy veins in the leg.
Key Benefits of VenaSeal™
VenaSeal™ offers several distinct advantages over traditional varicose vein treatments:
- No Anesthesia or Needle Sticks: Unlike some other treatments that require tumescent anesthesia involving multiple needle sticks, VenaSeal™ is virtually painless and does not involve injecting anesthesia into the leg.
- No Pre-Procedural Drugs: Patients can return to their normal activities right after the treatment since there are no pre-procedure drugs involved.
- No Risk of Burns or Nerve Damage: Unlike heat-based procedures, VenaSeal™ eliminates the risk of skin burns or nerve damage, ensuring a safer experience.
- Minimal Post-Treatment Discomfort: In most cases, patients do not require post-treatment pain medication or uncomfortable compression stockings, making recovery more comfortable.
A Unique and Safe Approach
The VenaSeal closure system is the only non-tumescent, non-thermal, non-sclerosant procedure that employs a proprietary medical adhesive delivered endogenously to close the vein. This distinctive approach has several notable advantages:
- Nerve Injury Risk Reduction: Unlike thermal-based procedures, VenaSeal™ significantly reduces the risk of nerve injury, especially when treating the small saphenous vein.
- Clinical Safety and Efficacy: Clinical studies have consistently demonstrated that the VenaSeal™ procedure is both safe and effective in treating varicose veins.
If you’re seeking a safe, minimally invasive solution for varicose veins, the VenaSeal™ closure system could be the answer you’ve been looking for. With its unique medical adhesive approach, lack of anesthesia, and minimal post-treatment discomfort, VenaSeal™ stands out as a convenient and effective option for permanently treating varicose veins. Say goodbye to the discomfort of venous reflux disease and embrace a healthier, pain-free future with VenaSeal™.
“Bringing Experts Together for Unparalleled Vein and Vascular Care”
La Jolla Vein & Vascular (formerly La Jolla Vein Care) is committed to bringing experts together for unparalleled vein and vascular care.
Nisha Bunke, MD, Sarah Lucas, MD, and Amanda Steinberger, MD are specialists who combine their experience and expertise to offer world-class vascular care.
Our accredited center is also a nationally known teaching site and center of excellence.
For more information on treatments and to book a consultation, please give our office a call at 858-550-0330.
For a deeper dive into vein and vascular care, please check out our Youtube Channel at this link, and our website https://ljvascular.com
For more information on varicose veins and eliminating underlying venous insufficiency,
Please follow our social media Instagram Profile and Tik Tok Profile for more fun videos and educational information.
For more blogs and educational content, please check out our clinic’s blog posts!