Peripheral artery disease, also known as PAD affects 1 in 20 adults over the age of 50. Most people with PAD do not need a vascular procedure. However, it is extremely important to get an accurate diagnosis in order to make lifestyle changes and other interventions, to reduce your risks of worsening disease and complications like heart disease and stroke. Our doctors can help make an accurate assessment and give guidance to reduce your risks. Treatment may be recommended for severe cases of PAD, resulting in lifestyle limiting claudication, non-healing ulcers and ischemic rest pain.
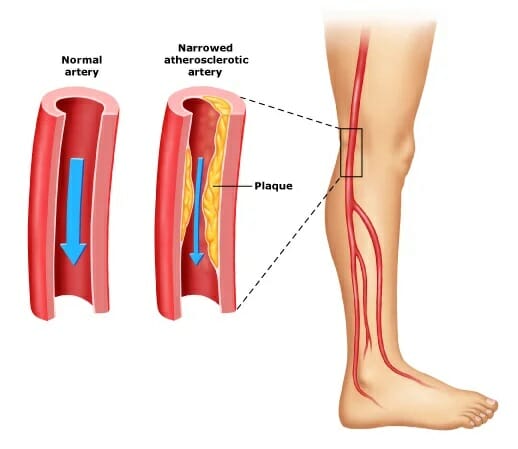
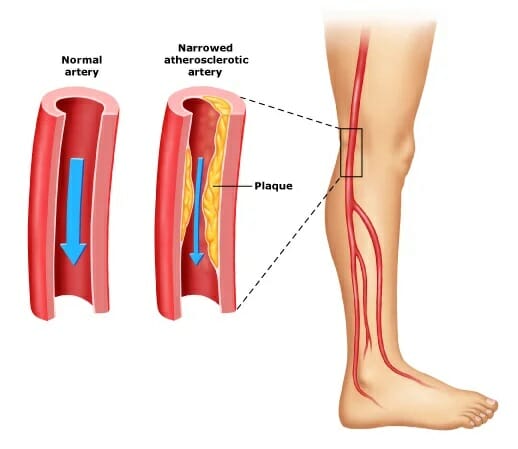
PAD develops when excessive plaque buildup on the artery walls, causing narrowing of the arteries. The arteries deliver oxygen-rich blood from the heart to other parts of the body. When plaque builds up, it usually restricts the flow of blood, oxygen, and glucose. The obstruction causes pain in the leg as the muscles and tissues are starved for oxygen and other nutrients from the blood. While the pain usually occurs in your legs primarily, it can also be felt in other parts of the body, including your arms, stomach, hip, head, and kidneys.
Are You at Risk for Peripheral Arterial Disease (PAD)?
In most cases, the PAD symptoms are on the lower extremities. You may experience some pain, craping, or tiredness in your hip or leg muscles when climbing stairs or walking. However, the pain usually goes away with rest, only to resurface when you start walking again. Individuals suffering from peripheral arterial disease are at a high risk of coronary artery disease, stroke, or heart attack. Even worse, if left untreated, the condition can lead to gangrene and amputation.
Peripheral Arterial Disease – Diagnosis
At La Jolla Vein & Vascular, we have highly trained physicians who offer a comprehensive diagnosis to develop customized treatments of Peripheral artery disease (PAD). We understand that no two patients’ conditions are similar. Our full-service vascular lab provides state-of-the-art testing to ensure that our physicians address each patient case quickly and accurately. Our doctors and nurses also have broad experience in this field and use advanced tools to achieve limb-saving results even for challenging, impaired patients. Our PAD diagnosis procedure involves the following:
OUR PATIENTS SAY

Beautiful facility! I walked in without an appointment and they took me right away! It was even the end of the day…I was so grateful…Every single person was soooo pleasant! Super impressed ❤️
I am pleased to recommend La Jolla Vein & Vascular. I am in the process of receiving treatment there. The entire medical staff are super friendly, welcoming and very helpful. Everyone is courteous, including the physicians. I’ve had one doctor follow my case. He’s the one who always treats me at appointments and closely follows my health. I am very comfortable going there. Would go again if needed and encourage anyone who’s thinking of making an appointment to do so asap. You’ll see what a wonderful experience it is. It’s the people who make it so special!
Dr De Young is personable and thorough in his explanations. Exceptional.
The staff at La Jolla Vein Care Center are outstanding. They are friendly and helpful. Dr. Lucas and my ultrasound tech were both very thorough, kind and answered all of my questions. The new office was beautiful. I feel very confident that I am in good hands and that any up coming treatments will be successful. Thank for for making me feel so comfortable.
From my greeting at the front desk to the ultrasound and visit with the doctor, I received excellent care. It’s clear they care about their patients and all the staff couldn’t have been nicer or more helpful. I also appreciate how much time the doctor spent with me to explain the results and the next steps. I would definitely recommend this office to friends with vein issues.
The staff members that I interacted with were all professional, conscientious and empathetic to my complaints and discomfort. I was taken into the ultrasound room a few minutes before my appointment time. I did not have a long wait before the ultrasonographer came and ran the machine. It was also a short wait before Dr. Steinburg came into the room with a warm, welcoming smile. We discussed my ultrasound and the things I was experiencing . I scheduled another appointment for next year and was offered a bottle of water upon leaving the office. All in all, I thought it was a very satisfactory appointment.
Everyone here is so nice! Usually front desk medical personnel are so rude. The front desk ladies Alejandra, Anna, and I think her name is Liz, went above and beyond to take care of me and my insurance issues. The techs are great too! Rachel and a male technician assisted me…both of them implemented different techniques to make me feel more at ease during an uncomfortable and painful process. These procedures were rough…and I am grateful everyone was so sweet to me. Thanks again.
When I arrived for the first time, I could barely walk. My legs were red and swollen. After my treatments, I can now walk again. I’m so thankful to the doctor and his staff. They are caring, supporting and knowledgeable about my issues. Five Stars all the way!!!!
The staff kept you informed as to when you would be seen and the wait was not too long. Emily took care of my ultrasound and was very accommodating giving me an extra pillow and playing a video to watch. The office is very courteous and professional- Nadia answered our questions and offered us a bottle of water. I have been seeing Dr. Bunke, but now Dr. Lucas and will continue coming to La Jolla Vein Care!
I had the best experience at La Jolla Vein Care. Dr.Bunke is an amazing doctor with the best bedside manners, she truly cares about her patients, she explained everything to me. My procedures where so easy I was impressed how painless and fast my appointments. Anna M was very helpful scheduling my treatments and checking on me to make sure all of my questions were answered. I am very pleased thank you !!! I truly recommend La Jolla Vein Care!
The office is exceptional, from front desk, to exam staff to the physicians. They have created a welcoming, relaxing environment, and take their time in examining and consulting with you to provide the best outcome. I highly recommend La Jolla Vein & Vascular for the assessment and treatment of your vein and vascular function.
La Jolla Vein care has the best staff ever. They are so nice, accommodating and professional!! Dr. Bunke is the best doctor that I ever seen. She is so friendly upfront and has the best bed side manner. I thank this office for letting me be their patient. 💜. Plus they are so careful with COVID which I really appreciate!!!
I have been having leg treatments for several months now La Jolla Vein Care. Every time I go to an appointment; the staff is so friendly and takes such good care of me; always informative; not in a rush and always friendly (especially Alejandra & Anna to name a few). Of course Dr. Lucas is amazing. The treatments have changed my life. Overall this has been an incredible experience.
We were early and didn’t have to wait at all. The tech that did my husband’s ultrasound, Monica, was very accommodating with my husband’s Parkinson’s. Doctor Lucas whom we hadn’t seen before, came to us instead of making my husband walk down to another office. She spent a lot of time getting caught up on Steve’s background issues/conditions. I was impressed by this medical group before, so I was surprised that the staff was even better this time around; I honestly didn’t think there was room for improvement!
Highly recommend! Entire staff are warm& friendly, professional and accommodating. The doctor took the time to thoroughly explain everything and encouraged me to ask questions. I never felt rushed. Significantly better experience than the other 2 vein clinics I’ve been to on the east coast. I wish I could’ve just come here from the beginning.
To make an appointment or to inquire about how we can help you understand your treatment options
La Jolla – Text us or Call 858-550-0330
Vista – Text us or Call 760-249-7007




























