From Discomfort to Confidence: Patient Transformation Stories in Varicose Vein Treatment
LJVascular2024-10-23T18:24:00-07:00From Discomfort to Confidence: Patient Transformation Stories in Varicose Vein Treatment
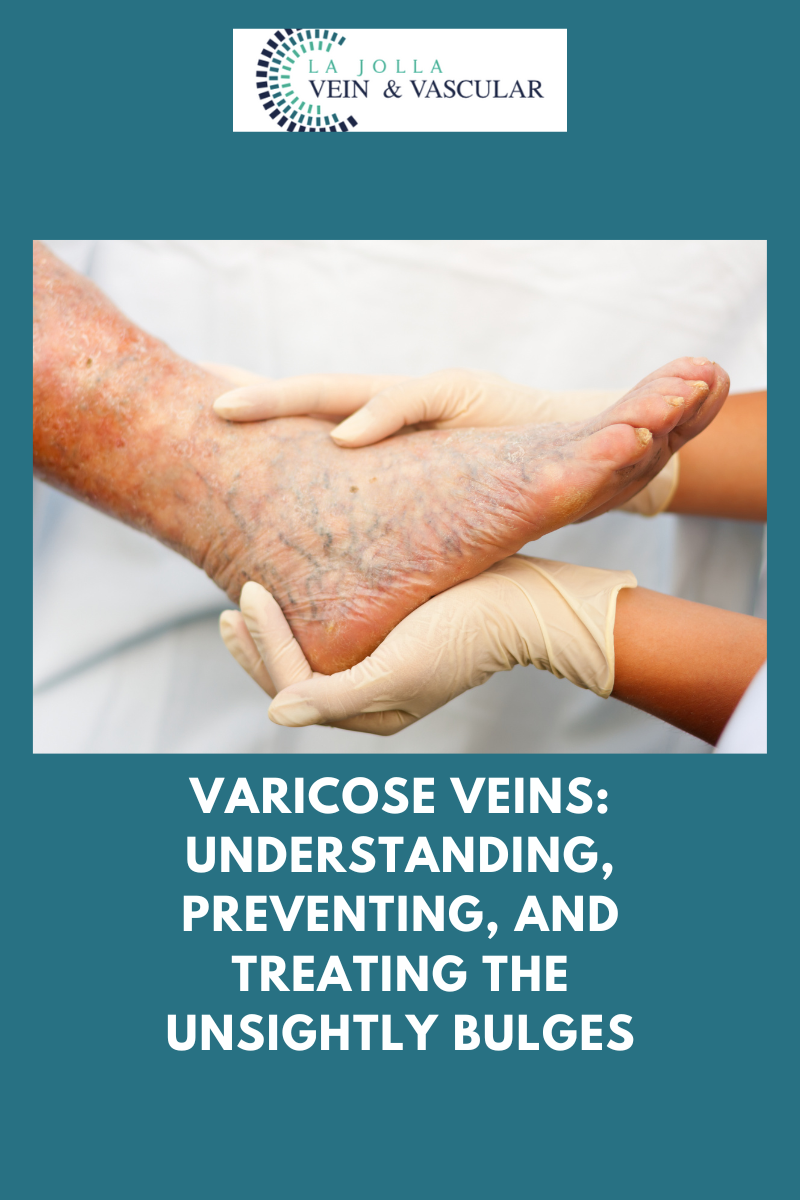
Varicose veins, those unsightly, swollen veins lurking just beneath the skin’s surface, can be a cause for concern among many individuals. While they most commonly make their appearance on the legs, these pesky veins can manifest elsewhere in the body. In this blog post, we’ll take a deep dive into the world of varicose veins, unraveling their nature, exploring their root causes, and shedding light on potential avenues for relief.
Unraveling the Mystery of Varicose Veins
Varicose veins result from veins that have become swollen and twisted, creating a visible presence just below the skin’s surface. Their appearance may raise alarm bells, but it’s important to note that they are a widespread condition affecting numerous people. These veins can frequently bring about discomfort, pain, or a sensation of heaviness in the legs.
Delving into the Culprits Behind Varicose Veins
The primary instigator behind varicose veins is malfunctioning vein valves. These valves play a crucial role in ensuring proper blood circulation by allowing blood to travel upward towards the heart and preventing it from pooling within the veins. When these valves fail to do their job, blood accumulates within the veins, causing them to stretch and enlarge. This condition is typically attributed to venous reflux disease, which also goes by the names venous stasis, venous insufficiency, or venous incompetence.
The Mechanism of Venous Reflux
Venous reflux, a phenomenon where blood flows backward against gravity due to faulty valves, is at the heart of varicose vein formation. Normally, the calf muscles assist in pumping blood upwards, but when valves fail, blood tends to accumulate in the lower legs, leading to visible bulging of the veins. This condition is most commonly observed in the great and small saphenous veins, which play a pivotal role in returning blood from the legs to the heart. Remarkably, over 90% of leg-related varicose vein cases are linked to these veins.
Evidential Insights from Our Research
A significant study led by Dr. Nisha Bunke and published in the Journal of Vascular Ultrasound in 2018 examined over 1,000 legs afflicted with varicose veins. The findings revealed that the great and small saphenous veins were predominant contributors to varicose veins in a majority of cases. The Great Saphenous Vein (GSV), coursing through the middle of the thigh and calf, and the Small Saphenous Vein (SSV), situated along the back of the calf, were especially implicated.
Discovering Viable Treatment Options
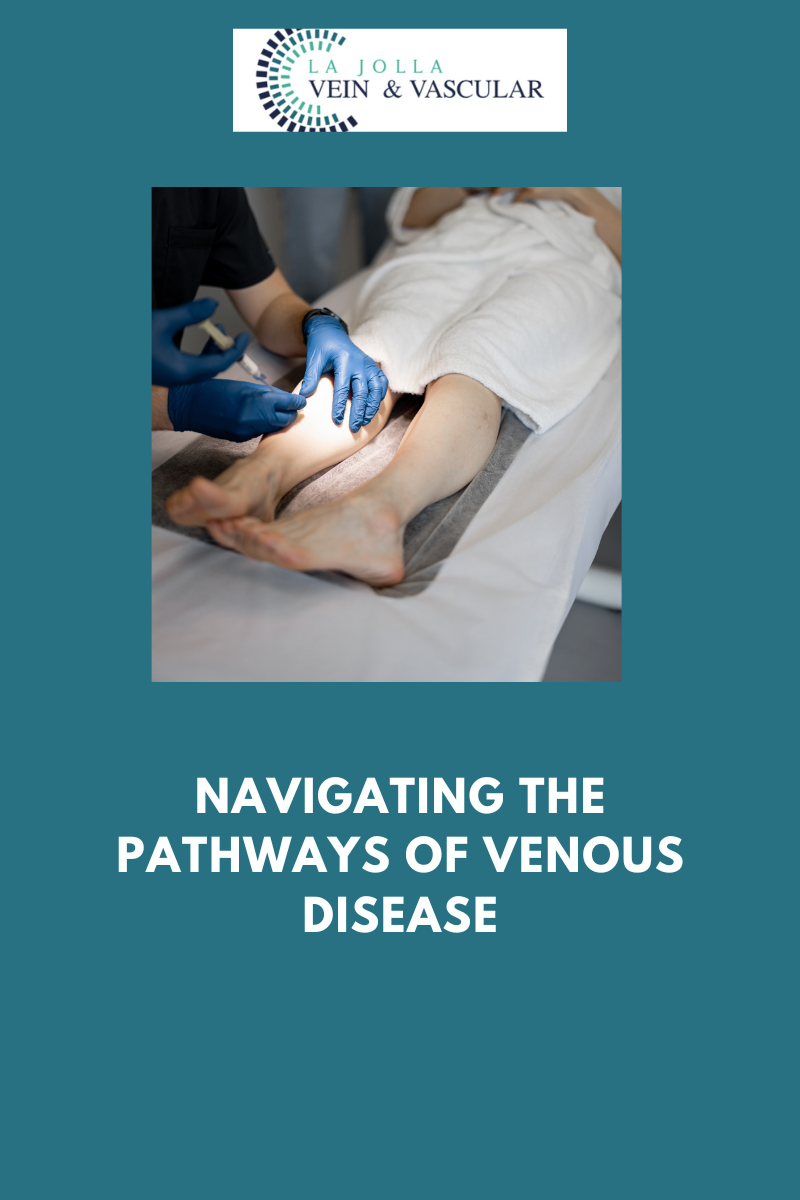
The good news is that varicose veins need not be a condition without recourse. Thanks to advancements in medical technology and knowledge, a range of treatment options exists to alleviate discomfort and enhance the appearance of affected veins. Numerous minimally invasive procedures, such as laser ablation, radiofrequency ablation, and sclerotherapy, have proven their efficacy in addressing varicose veins.
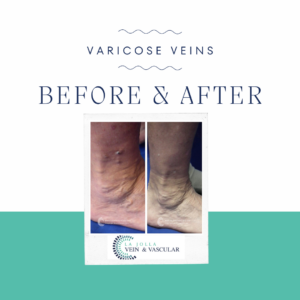
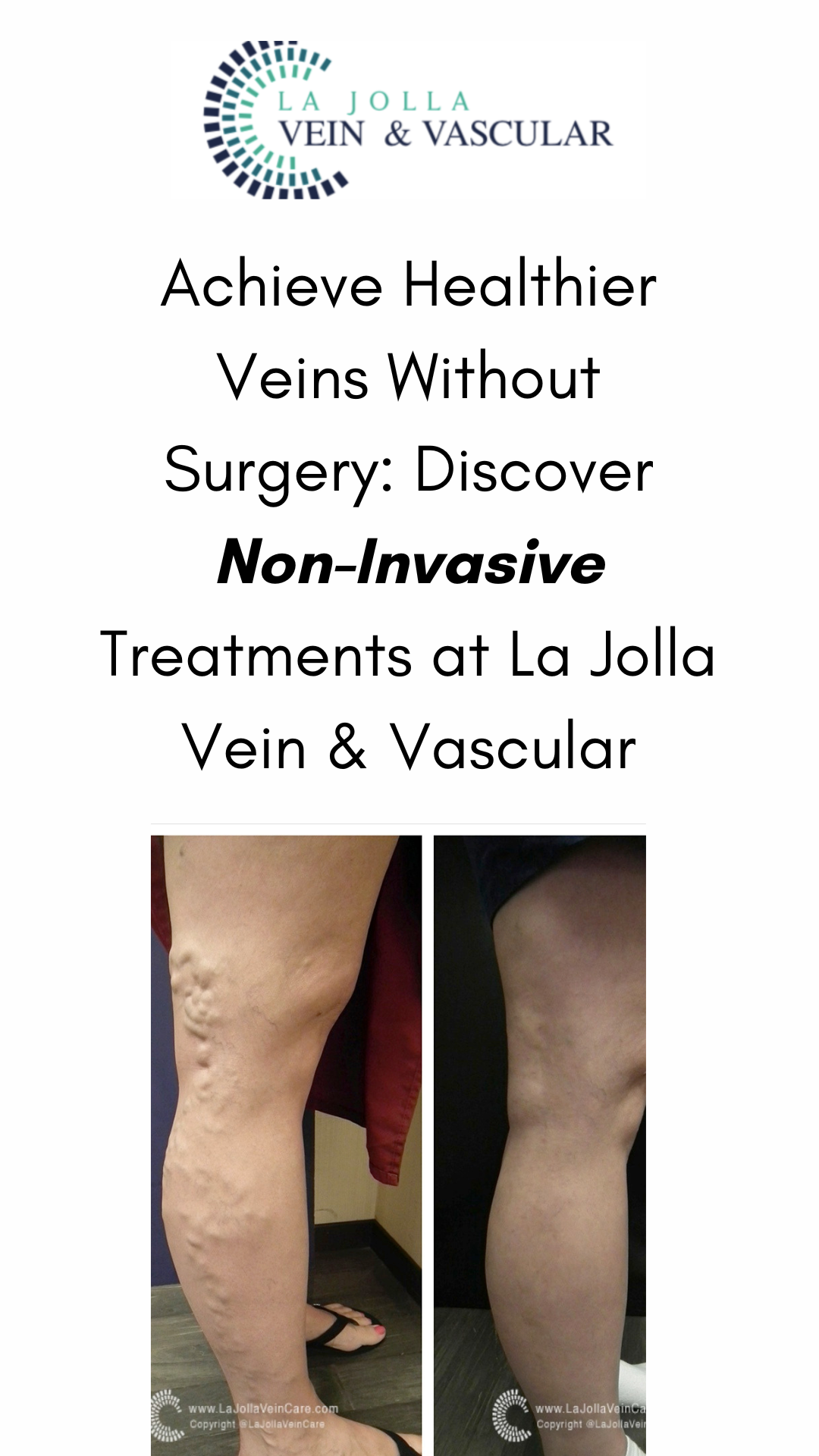
A Visual Testament to Transformation

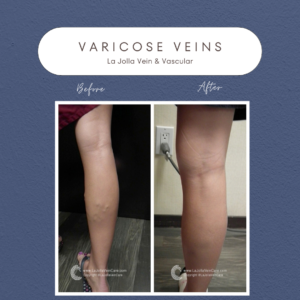
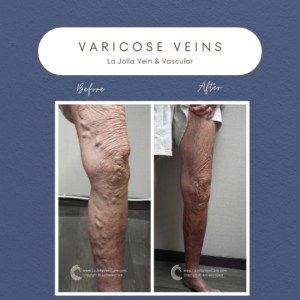
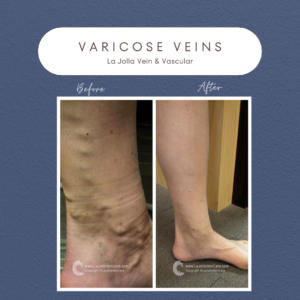
Witnessing the transformative outcomes of varicose vein treatment can be truly remarkable. Many individuals undergo significant improvements in both the appearance of their veins and the symptoms they experience. Before-and-after images serve as tangible evidence of the positive impact that appropriate treatment can have on one’s vascular health and overall well-being.
While varicose veins are a common condition, understanding their origins and potential treatment options empowers individuals to take charge of their vascular health. With modern medical techniques, those grappling with varicose veins can seek relief and experience a substantial enhancement in their quality of life. Whether it involves comprehending the role of malfunctioning vein valves, delving into the intricacies of venous reflux, or exploring diverse treatment modalities, the journey to healthier veins starts with education and awareness.
“Bringing Experts Together for Unparalleled Vein and Vascular Care”
La Jolla Vein & Vascular (formerly La Jolla Vein Care) is committed to bringing experts together for unparalleled vein and vascular care. Nisha Bunke, MD, Sarah Lucas, MD, and Amanda Steinberger, MD are specialists who combine their experience and expertise to offer world-class vascular care. Our accredited center is also a nationally known teaching site and center of excellence.
For more information on treatments and to book a consultation, please give our office a call at 858-550-0330.
For a deeper dive into vein and vascular care, please check out our Youtube Channel at this link, and our website https://ljvascular.com
For more information on varicose veins and eliminating underlying venous insufficiency,
Please follow our social media Instagram Profile and Tik Tok Profile for more fun videos and educational information.
For more blogs and educational content, please check out our clinic’s blog posts!