Why do Varicose Veins occur?
LJVascular2024-07-06T16:37:07-07:00Unveiling Key Insights: Your Comprehensive Guide to Understanding Varicose Veins
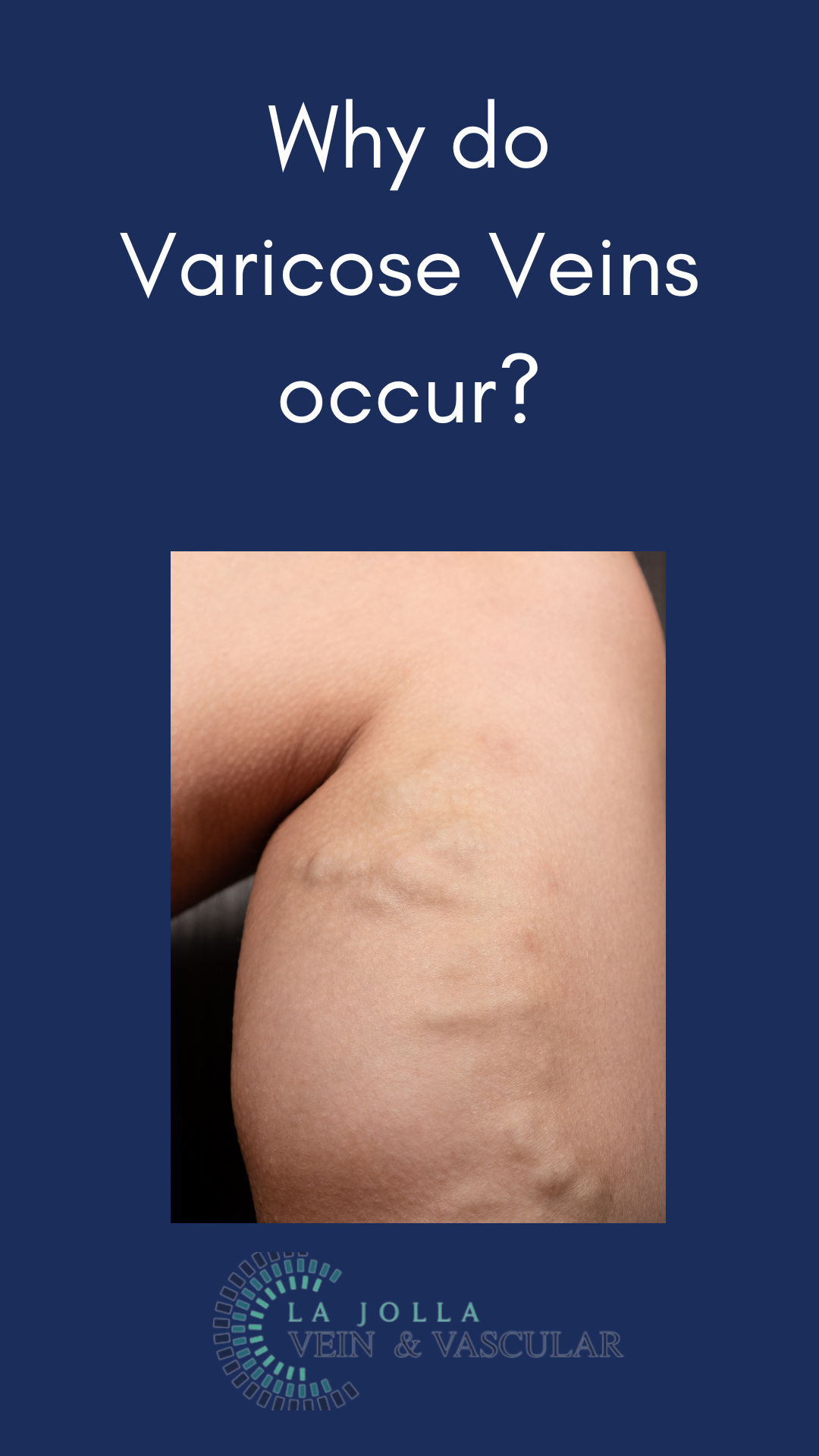
Varicose veins, those twisted and bulging veins beneath the skin’s surface, affect numerous individuals, often causing discomfort and aesthetic worries. This informative blog post aims to explore the intricacies of varicose veins and the underlying venous reflux disease. From comprehending the causes to investigating symptoms and potential treatments, let’s embark on a journey toward vein health and relief.
Understanding Varicose Veins
Easily visible on the skin’s surface, particularly in the legs, varicose veins are swollen and twisted veins. Despite their commonality, these veins can induce pain and aesthetic concerns, underscoring the importance of proper understanding and treatment.
Identifying the Culprits: Causes of Varicose Veins
The primary cause of varicose veins resides in malfunctioning vein valves, leading to blood accumulation within the veins. This pooling causes the veins to stretch and expand, resulting in their distinctive appearance. Venous reflux disease, known as venous stasis, venous insufficiency, or venous incompetence, is a prevalent underlying condition contributing to varicose veins. This condition involves the backward flow of blood in deep and/or superficial leg veins.
Insights from Research
Dr. Nisha Bunke, spearheading our study published in the Journal of Vascular Ultrasound in 2018, scrutinized over 1,000 legs with varicose veins. The study underscored that a significant majority—over 90%—of varicose vein sources were the great and small saphenous veins. The Great Saphenous Vein (GSV) courses through the middle of the thigh and calf, while the small saphenous vein (SSV) travels along the back of the calf.
Unraveling Symptoms
Varicose veins and venous reflux disease present an array of symptoms, including aching, tenderness, heaviness, fatigue, restlessness in the legs, burning and throbbing pain, itching, leg cramps (especially at night), ankle swelling, skin discoloration, and even skin ulcers above the ankle. Left untreated, complications such as painful vein inflammation (superficial phlebitis), blood clots within varicose veins (superficial thrombophlebitis), and skin issues like discoloration, eczema, or ulcers may arise.
The Importance of Ultrasound Diagnosis
Duplex ultrasound technology is crucial for effective diagnosis, evaluating veins beneath the skin’s surface. This technology detects leaky valves, determines blood flow direction, and identifies blockages or scars within veins, providing essential information for tailored treatment plans.
Customized Treatment Approach
Comprehensive treatment of varicose veins involves multiple steps:
Step 1: Addressing the Root Issue
Effective treatment begins with targeting venous reflux, often focusing on the saphenous veins, the common source of the problem. Innovative vein ablation procedures like radiofrequency ablation (RFA), laser ablation, mechanico-chemical ablation (MOCA), and Varithena Foam are employed to restore proper blood flow.
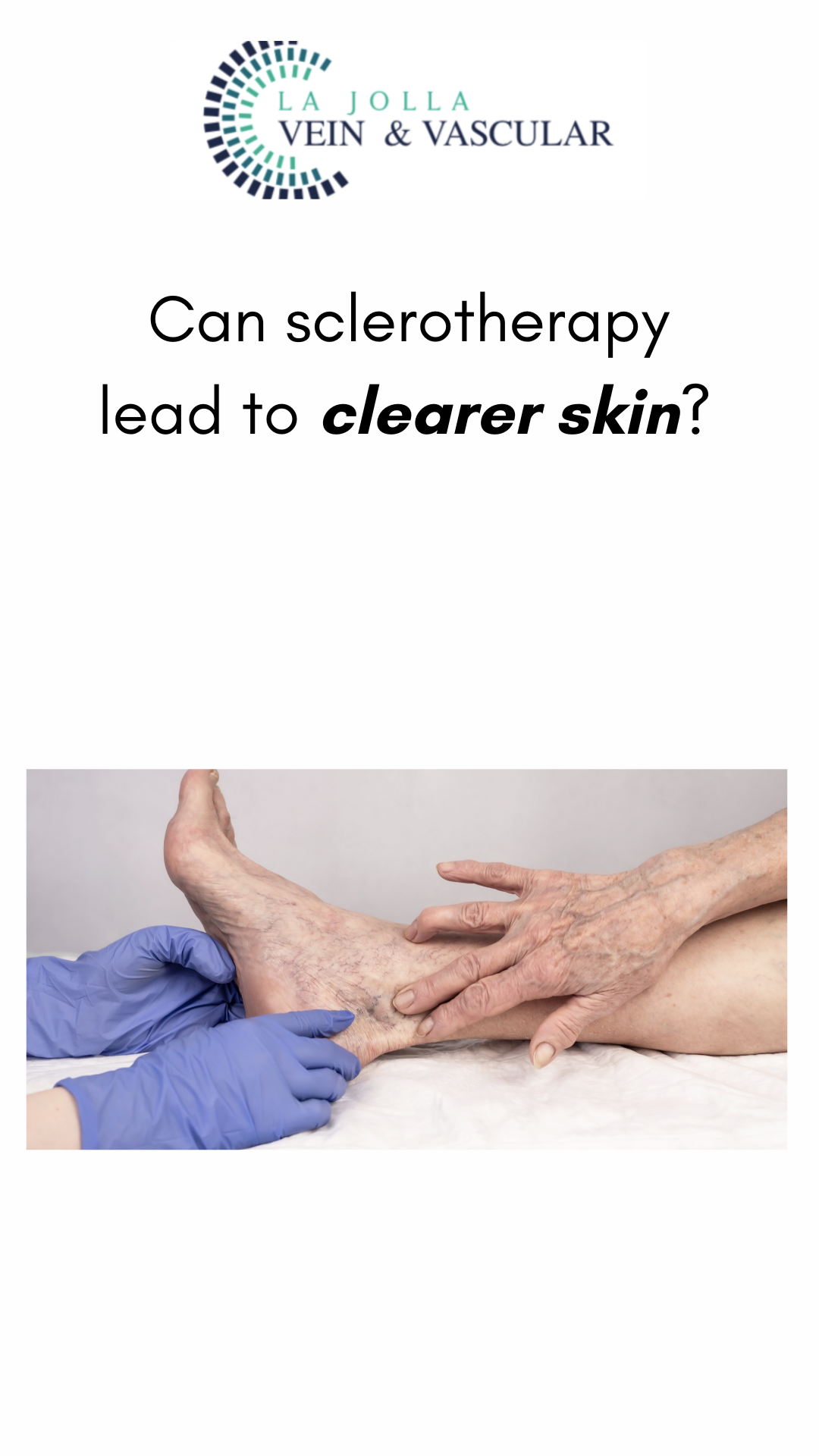
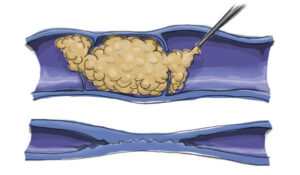
Step 2: Managing Varicose Veins
Post successful treatment of underlying reflux, attention shifts to managing varicose veins. Methods like foam sclerotherapy, injecting foamed medication to cause scarring and eventual vein dissolution, and phlebectomy involving tiny incisions to remove veins, are commonly employed.
Varicose veins and venous reflux disease impact numerous lives, causing discomfort and concern. By comprehending their causes, identifying symptoms, and exploring innovative varicose vein treatments, individuals can take control of their vein health. At La Jolla Vein & Vascular, we’re committed to providing personalized care and effective solutions to alleviate symptoms and enhance the quality of life. If you’re ready to embark on the journey toward healthier veins, contact us today and take the initial step toward lasting relief and wellness.
“Bringing Experts Together for Unparalleled Vein and Vascular Care”
La Jolla Vein & Vascular (formerly La Jolla Vein Care) is committed to bringing experts together for unparalleled vein and vascular care.
Nisha Bunke, MD, Sarah Lucas, MD, and Amanda Steinberger, MD are specialists who combine their experience and expertise to offer world-class vascular care.
Our accredited center is also a nationally known teaching site and center of excellence.
For more information on treatments and to book a consultation, please give our office a call at 858-550-0330.
For a deeper dive into vein and vascular care, please check out our Youtube Channel at this link, and our website https://ljvascular.com
For more information on varicose veins and eliminating underlying venous insufficiency,
Please follow our social media Instagram Profile for more fun videos and educational information.
For more blogs and educational content, please check out our clinic’s blog posts!