Exploring Upper Extremity Venous Study: A Vital Tool in Vascular Health
LJVascular2024-07-06T22:32:45-07:00Exploring Upper Extremity Venous Study: A Vital Tool in Vascular Health
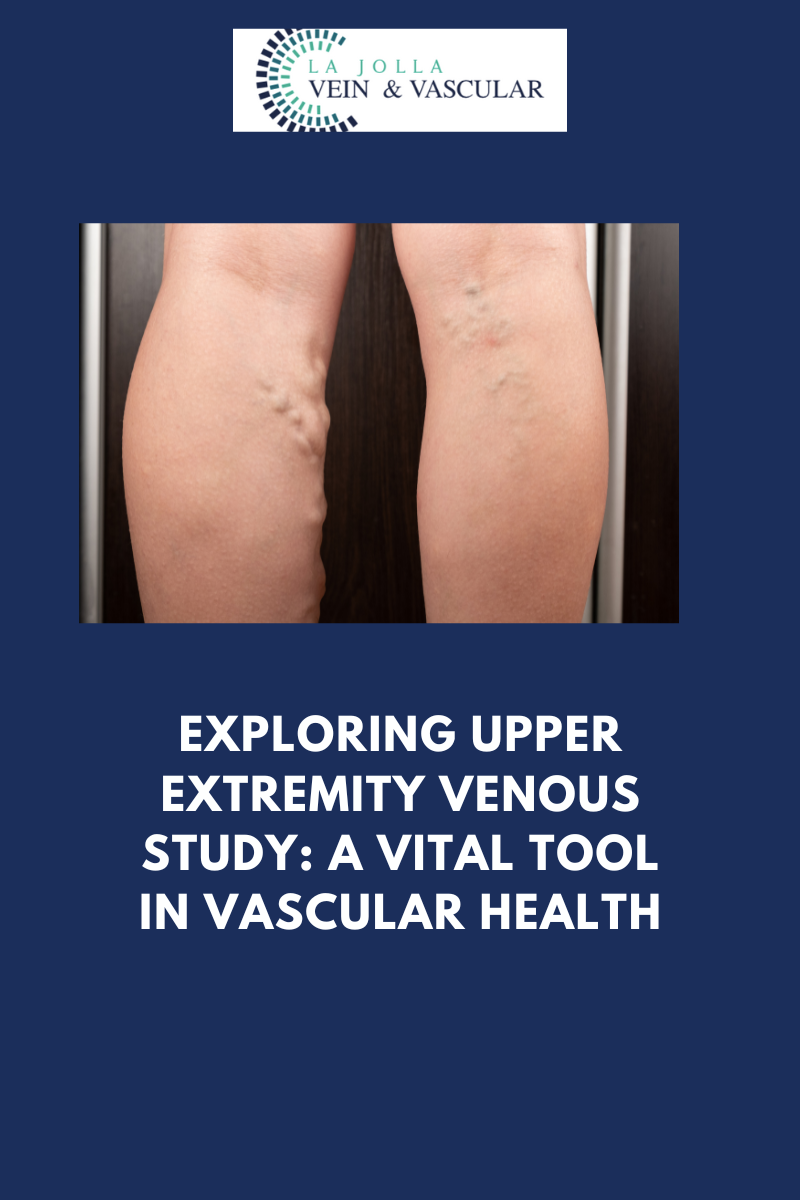
While deep vein thrombosis (DVT) in the legs often garners significant attention, it’s of paramount importance not to disregard the upper extremities when evaluating vein health. Enter the Upper Extremity Venous Study, a specialized ultrasound examination that assumes a pivotal role in unveiling potential issues in the arms and neck. In this blog post, we will delve into the significance of this study, its objectives, and the role it plays in diagnosing arm-related concerns.
Deciphering the Upper Extremity Venous Study
The Upper Extremity Venous Study stands as a non-invasive imaging procedure with a dedicated focus on the veins residing in the upper arms and neck. Its primary mission is to thoroughly assess both the deep and superficial venous systems in these anatomical regions. This study takes center stage when an individual presents specific signs and symptoms, particularly pain and swelling in the arms, demanding careful investigation.
Why is an Upper Extremity Venous Study Conducted?
Numerous factors prompt healthcare providers to recommend the performance of an Upper Extremity Venous Study:
- Arm Pain and Swelling: When a person experiences pain and swelling in one or both arms, especially if these symptoms remain unexplained or persistent, the Upper Extremity Venous Study proves invaluable in discerning the underlying causes.
- Evaluation of Venous Health: Just as the lower extremities demand scrutiny for the presence of DVT, it is equally imperative to inspect the upper extremities for potential venous irregularities. This study is instrumental in identifying conditions such as deep vein thrombosis, superficial vein complications, and more.
- Unexplained Symptoms: Occasionally, arm pain and swelling may manifest without an apparent cause. The Upper Extremity Venous Study, therefore, serves as a potent diagnostic tool to unveil concealed vascular concerns that might be at play.
The Procedure Unveiled
An Upper Extremity Venous Study is a procedure that adheres to a straightforward series of steps:
- Preparation: For this examination, no specialized preparation is necessary. Patients can typically maintain their regular routines, including eating, drinking, and taking prescribed medications.
- Application of Ultrasound Gel: A trained healthcare professional known as a sonographer will apply a specialized ultrasound gel to the skin in the areas of focus, which usually encompass the upper arms and neck.
- Transducer Deployment: The procedure employs a handheld device known as a transducer, which emits high-frequency sound waves. These waves engage with the blood vessels within the arms and neck, generating echoes that are subsequently translated into images.
- Real-Time Imaging: The transducer is maneuvered gently over the skin’s surface, affording real-time visualization of the veins in the upper extremities. This process unravels the veins’ structural details and facilitates an assessment of blood flow patterns.
The Upper Extremity Venous Study emerges as an invaluable instrument in the domain of vascular medicine. By comprehensively evaluating the deep and superficial venous systems within the arms and neck, it equips healthcare providers with the means to diagnose and address issues linked to arm pain, swelling, and other associated symptoms.
In the event that you, or someone within your purview, undergoes unexplained or persistent arm discomfort, seeking consultation with a healthcare provider and contemplating an Upper Extremity Venous Study can serve as an illuminating journey into the root causes. Early detection and intervention may pave the way for effective treatment and a brighter outlook for your arms.
“Bringing Experts Together for Unparalleled Vein and Vascular Care”
La Jolla Vein & Vascular (formerly La Jolla Vein Care) is committed to bringing experts together for unparalleled vein and vascular care.
Nisha Bunke, MD, Sarah Lucas, MD, and Amanda Steinberger, MD are specialists who combine their experience and expertise to offer world-class vascular care.
Our accredited center is also a nationally known teaching site and center of excellence.
For more information on treatments and to book a consultation, please give our office a call at 858-550-0330.
For a deeper dive into vein and vascular care, please check out our Youtube Channel at this link, and our website https://ljvascular.com
For more information on varicose veins and eliminating underlying venous insufficiency,
Please follow our social media Instagram Profile and Tik Tok Profile for more fun videos and educational information.
For more blogs and educational content, please check out our clinic’s blog posts!