Navigating vascular health: Insights to Ultrasound-Guided Foam Sclerotherapy
LJVascular2024-10-31T21:52:06-07:00Navigating Vascular Health: Insights to Ultrasound-Guided Foam Sclerotherapy

Ultrasound-Guided Foam Sclerotherapy: Elevating Vein Health
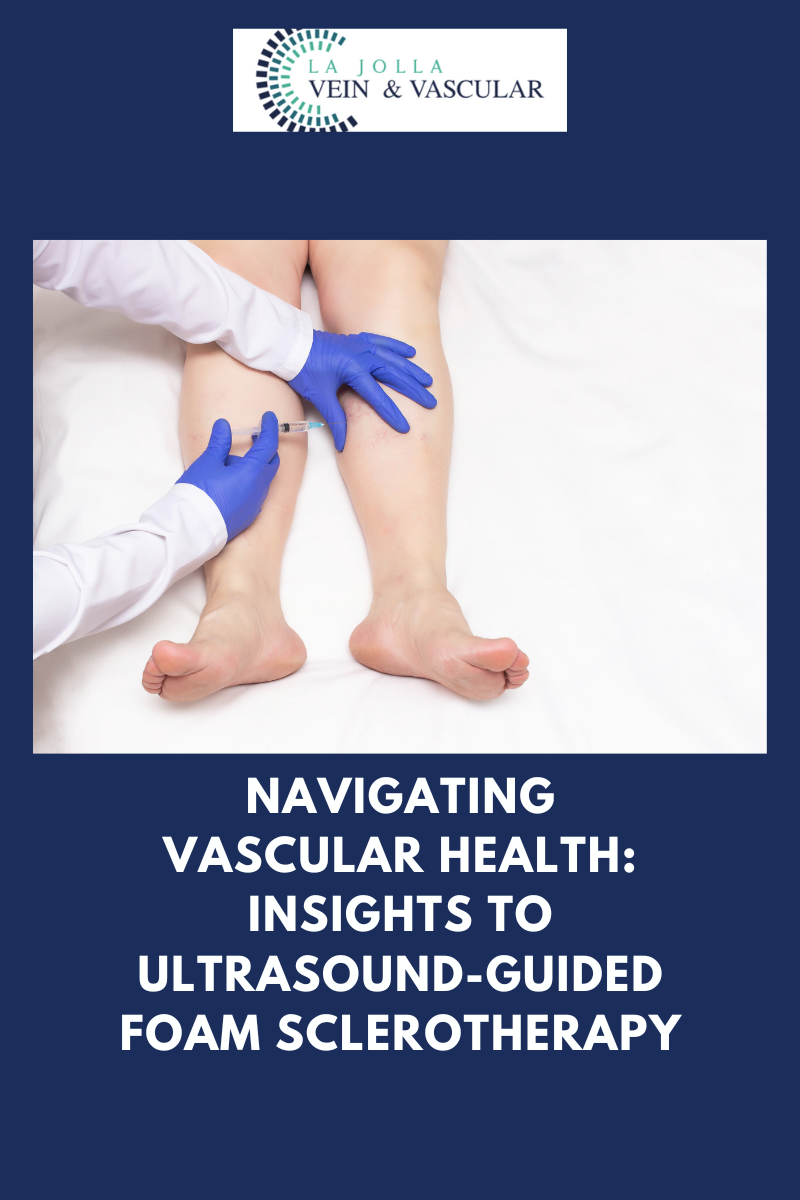
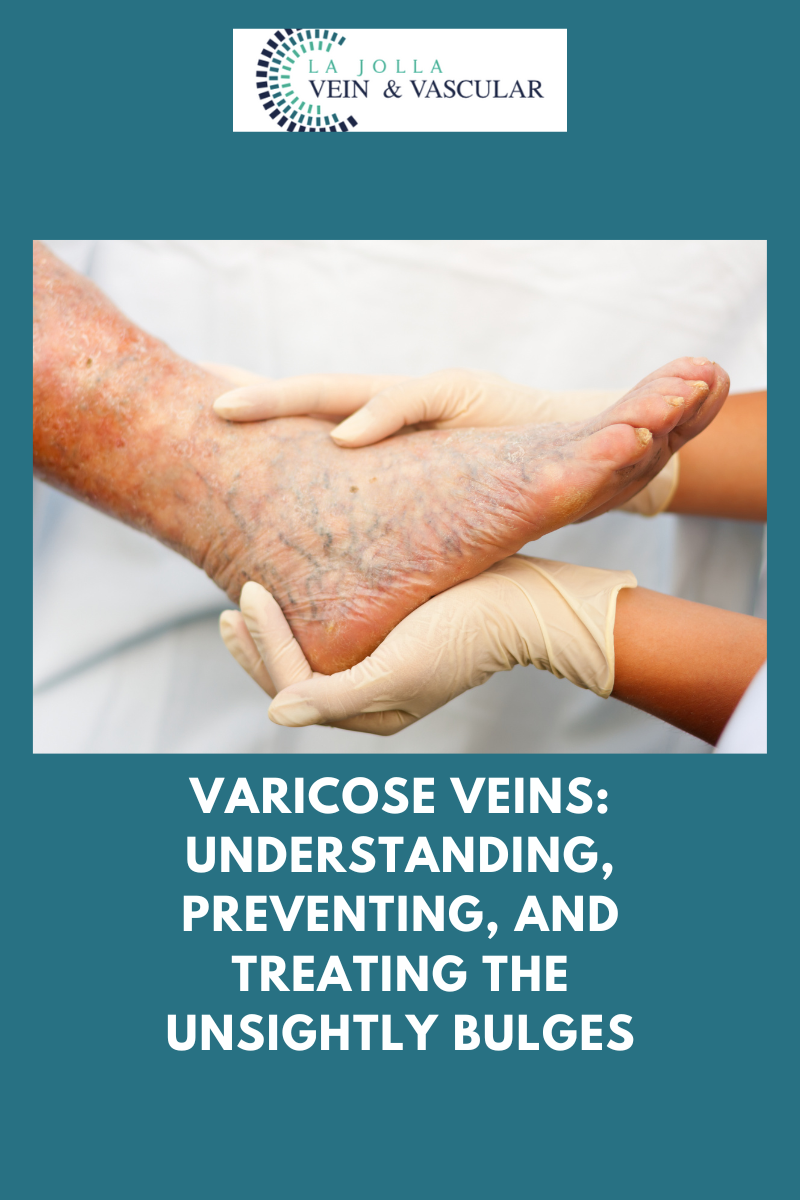
When it comes to combating surface varicose veins and those that remain hidden to the naked eye, the prowess of ultrasound-guided foam sclerotherapy shines. This advanced technique combines precise administration with ultrasound visualization, offering a safe and effective solution for various vein conditions. In this article, we delve into the details of ultrasound-guided foam sclerotherapy, the role of polidocanol (Asclera®), treatment frequency, and what you can expect on your treatment days.
Unveiling Ultrasound-Guided Foam Sclerotherapy: A Cutting-Edge Solution
Ultrasound-guided foam sclerotherapy harnesses the power of technology and medical expertise to target varicose veins that may not be immediately visible. The foam medication, guided by ultrasound, is precisely directed toward nearby varicose veins. This technique is not only effective for veins near the skin or nerves but also navigates veins with complex twists and turns.
Polidocanol (Asclera®): A Preferred Sclerosant
In the realm of sclerosant medications, polidocanol, under the brand name Asclera®, stands out as a preferred choice. Its comfort for patients and minimal risk of side effects make it a prime candidate for treatment. As a detergent-type medication, polidocanol gently disrupts the inner lining of veins. This action halts blood flow, eventually leading to the complete closure of the vein. Polidocanol, approved by the FDA since 2010 for varicose vein treatment, has a substantial track record of success in Europe for decades. The transformation of polidocanol into foam for treating larger veins, although an off-label use, has proven remarkably effective and well-tolerated by patients. Our seasoned experts at La Jolla Vein Care boast extensive experience in foam sclerotherapy, ensuring your vein health is in capable hands.
Treatment Frequency: A Personalized Approach
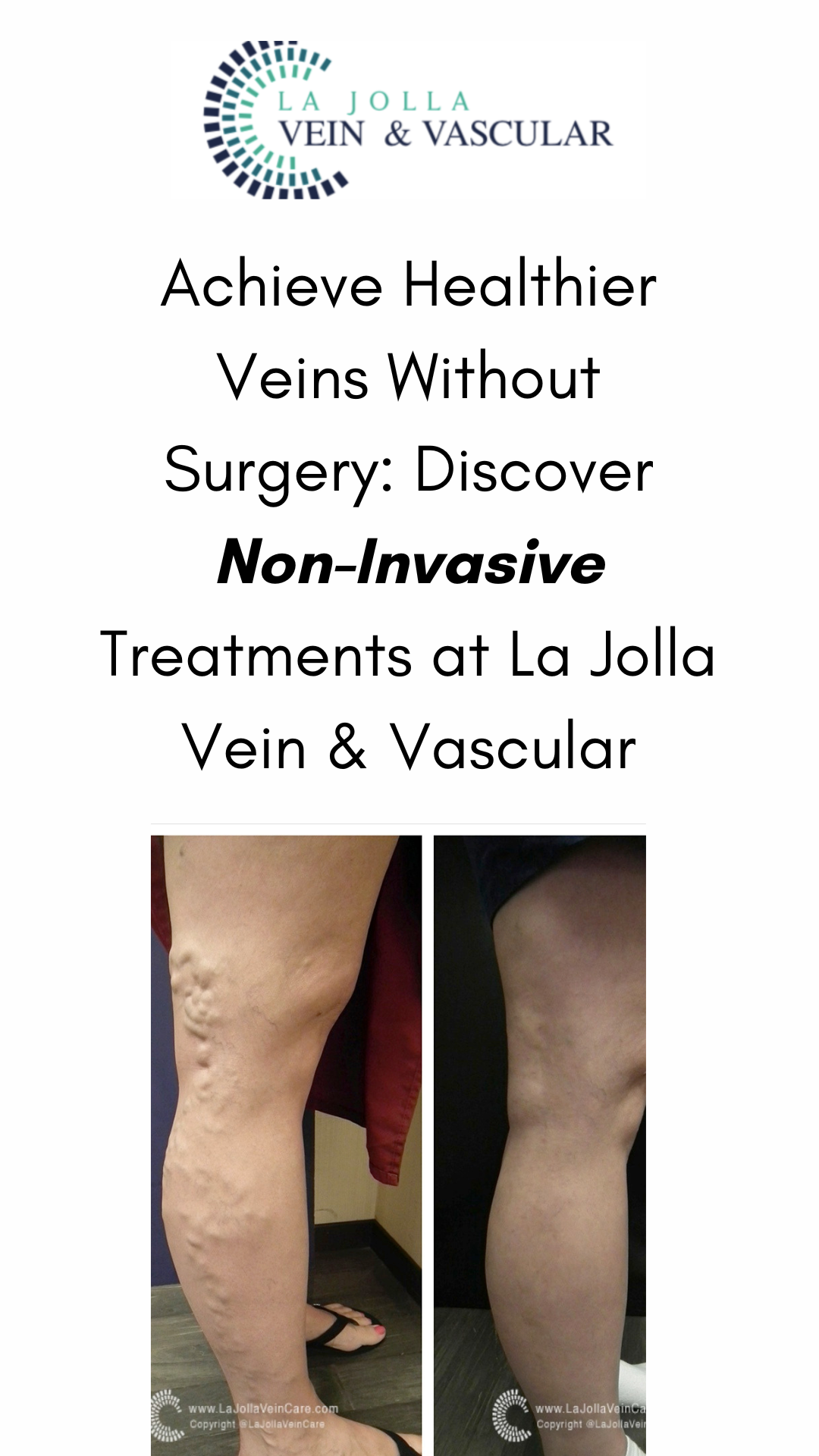
The number and frequency of treatments vary based on individual anatomy, vein response to treatment, and patient goals. On average, 2 to 5 treatment sessions achieve an 80% improvement. Some larger or stubborn veins may necessitate two or more sessions to achieve complete response.
Your Treatment Days: A Guided Journey to Vein Wellness
Preparing for your ultrasound-guided foam sclerotherapy treatment day is straightforward:
- Consent and Attire: You’ll sign a consent form and change into provided shorts.
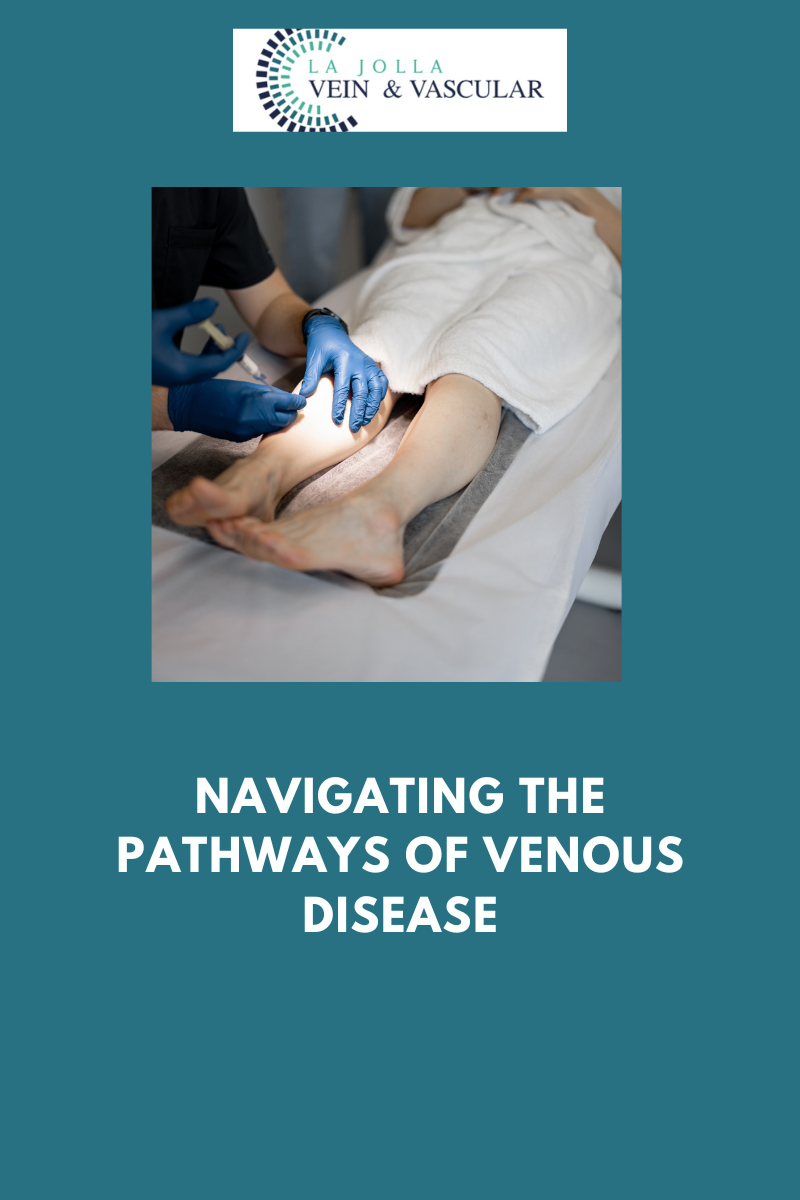
- Skin Preparation: Your skin will be cleaned with alcohol, and ultrasound will be used to locate the veins for targeted treatment.
- Injection Process: The foam medication will be injected into your veins using a fine needle, guided by ultrasound.
- Recovery Period: You’ll elevate your legs on a comfortable wedge pillow for around 15 minutes post-treatment.
- Compression Stockings and Walking: Following treatment, compression stockings will be applied, and you’ll walk for 30 minutes before departing. It’s normal to experience achiness and tenderness after treatment.
Ultrasound-guided foam sclerotherapy paves the way for enhanced vein health, offering precision and efficacy. At La Jolla Vein & Vascular, our dedicated medical team is committed to providing personalized care for your vein health journey. By embracing cutting-edge techniques like ultrasound-guided foam sclerotherapy, you’re embarking on a path to healthier, pain-free legs and elevated well-being.
Recommended fore you:
- A Comprehensive Guide to Ultrasound-Guided Foam Sclerotherapy (Before & After Treatment)
- Best Ultrasound Technician Team
“Bringing Experts Together for Unparalleled Vein and Vascular Care”
La Jolla Vein & Vascular (formerly La Jolla Vein Care) is committed to bringing experts together for unparalleled vein and vascular care.
Nisha Bunke, MD, Sarah Lucas, MD, and Amanda Steinberger, MD are specialists who combine their experience and expertise to offer world-class vascular care.
Our accredited center is also a nationally known teaching site and center of excellence.
For more information on treatments and to book a consultation, please give our office a call at 858-550-0330.
For a deeper dive into vein and vascular care, please check out our Youtube Channel at this link, and our website https://ljvascular.com
For more information on varicose veins and eliminating underlying venous insufficiency,
Please follow our social media Instagram Profile and Tik Tok Profile for more fun videos and educational information.
For more blogs and educational content, please check out our clinic’s blog posts!