How do I heal Leg Ulcers?
LJVascular2025-09-04T12:31:40-07:00Healing Leg Ulcers: Understanding, Treatment, and Prevention Strategies
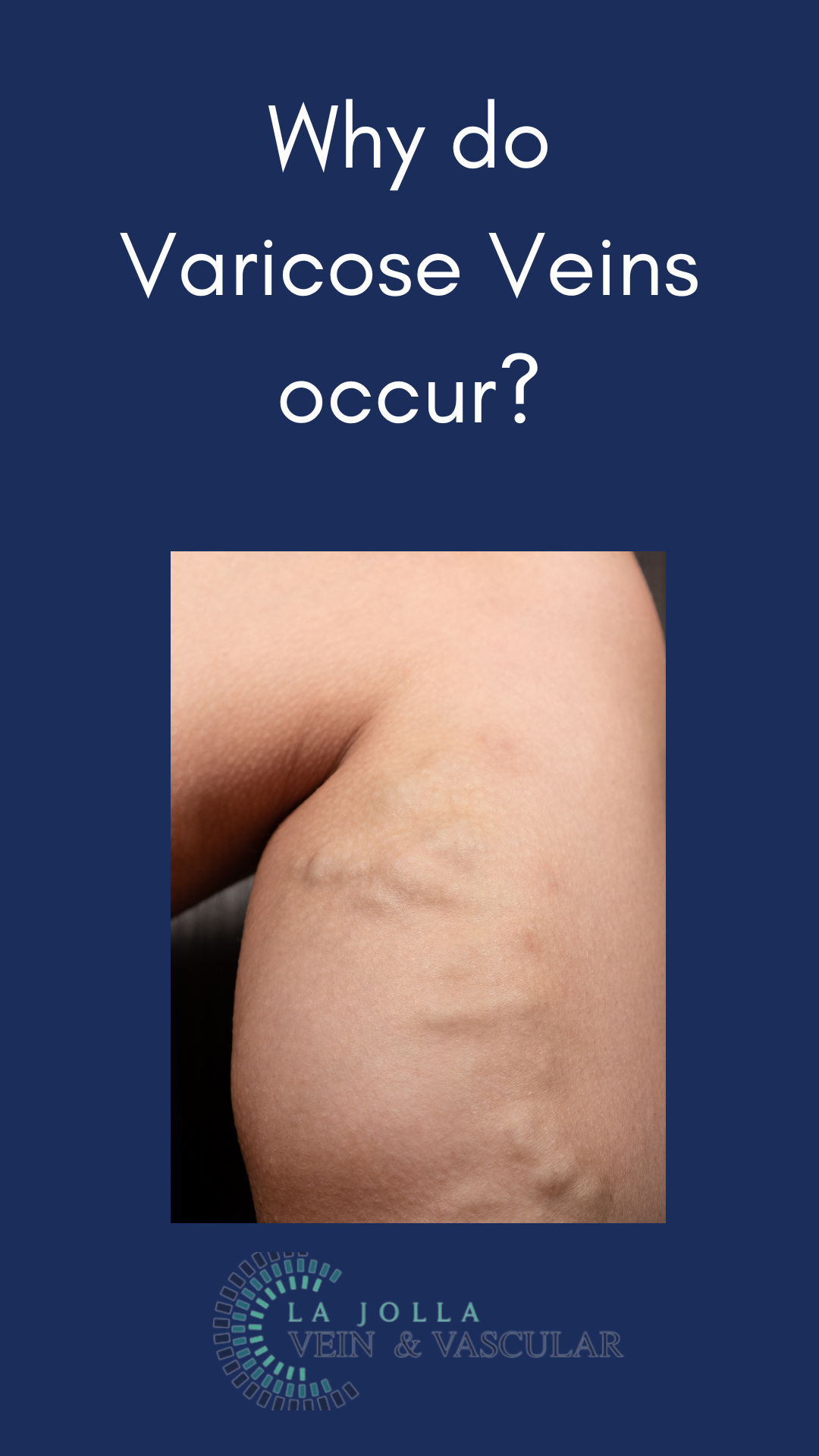
Within the sphere of vascular health, Chronic Venous Insufficiency (CVI) stands as a prevalent yet often misconstrued condition. Characterized by a cascade of symptoms that can ultimately result in skin changes and ulcers, CVI necessitates attention and effective management. In this article, we’ll […]