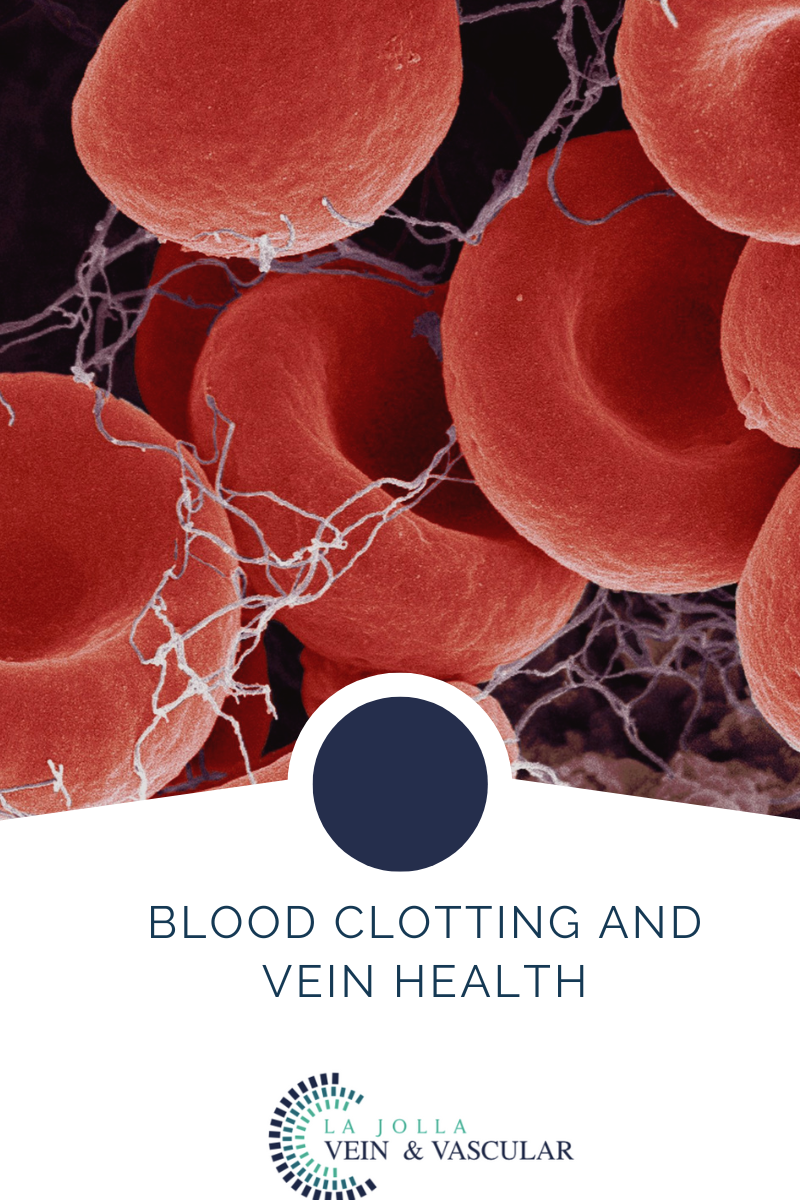
Blood Clotting & Vein Health
LJVascular2022-12-13T13:24:38-08:00When blood moves too slowly in your veins, it can cause a clump of blood cells (a blood clot or Thrombus). Deep vein thrombosis (DVT) is a condition in which a blood clot forms in the deep vein located in the leg, thigh, or pelvis. While Deep vein thrombosis (DVT) is common in […]