Unveiling the Magic of Sclerotherapy: Say Goodbye to Spider Veins
LJVascular2024-10-23T22:29:23-07:00Unveiling the Magic of Sclerotherapy: Say Goodbye to Spider Veins
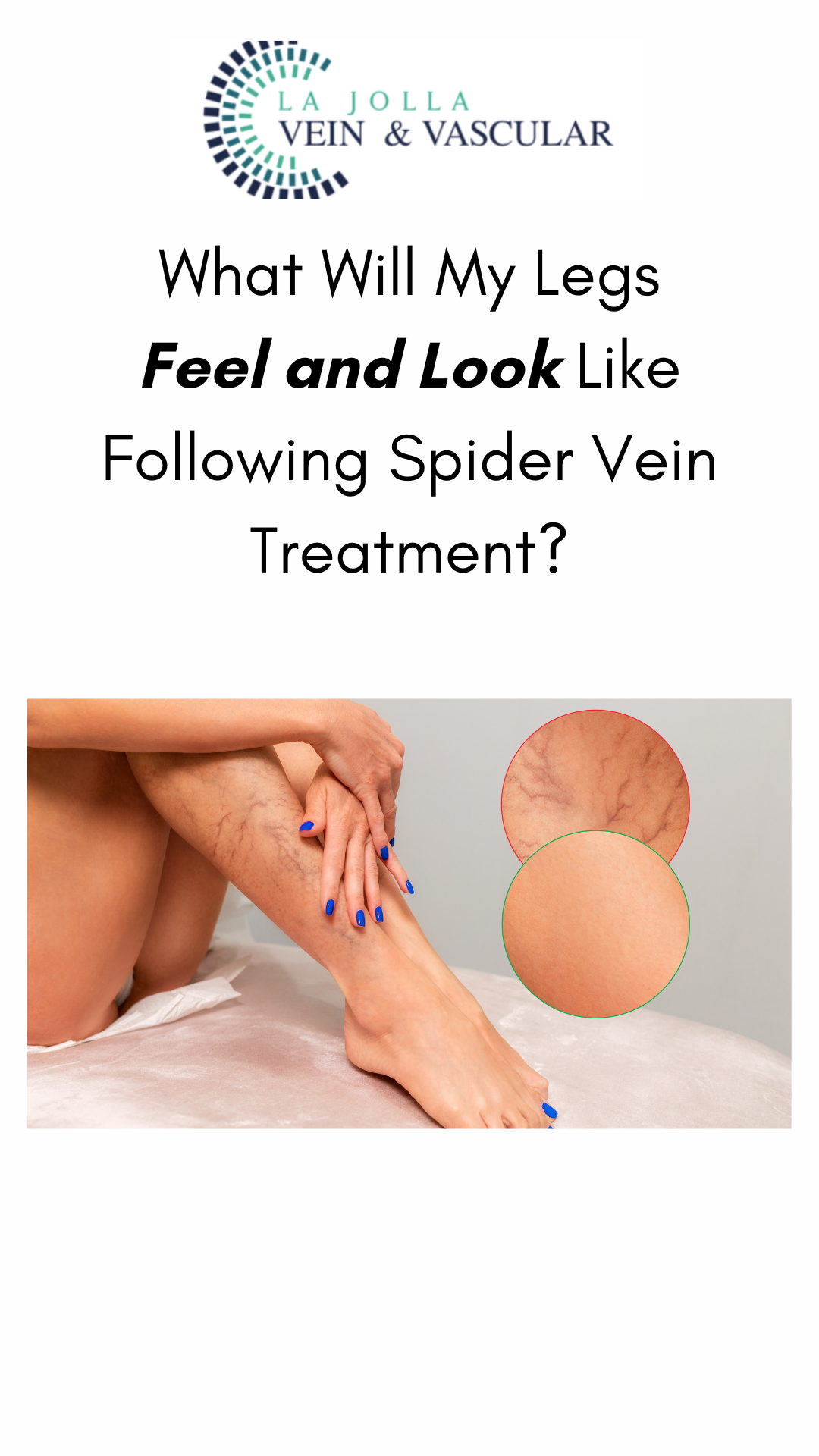
Are you tired of those pesky spider veins crisscrossing your legs, making you hesitate to show off your beautiful skin? If so, you’re not alone. Spider veins and reticular veins are common issues that many individuals face. But fear not; there’s a magical solution called sclerotherapy that can help you bid farewell to these unwelcome guests. In this blog post, we’ll unveil the wonders of sclerotherapy, from its procedure to what you can expect on your treatment days.
Understanding Sclerotherapy
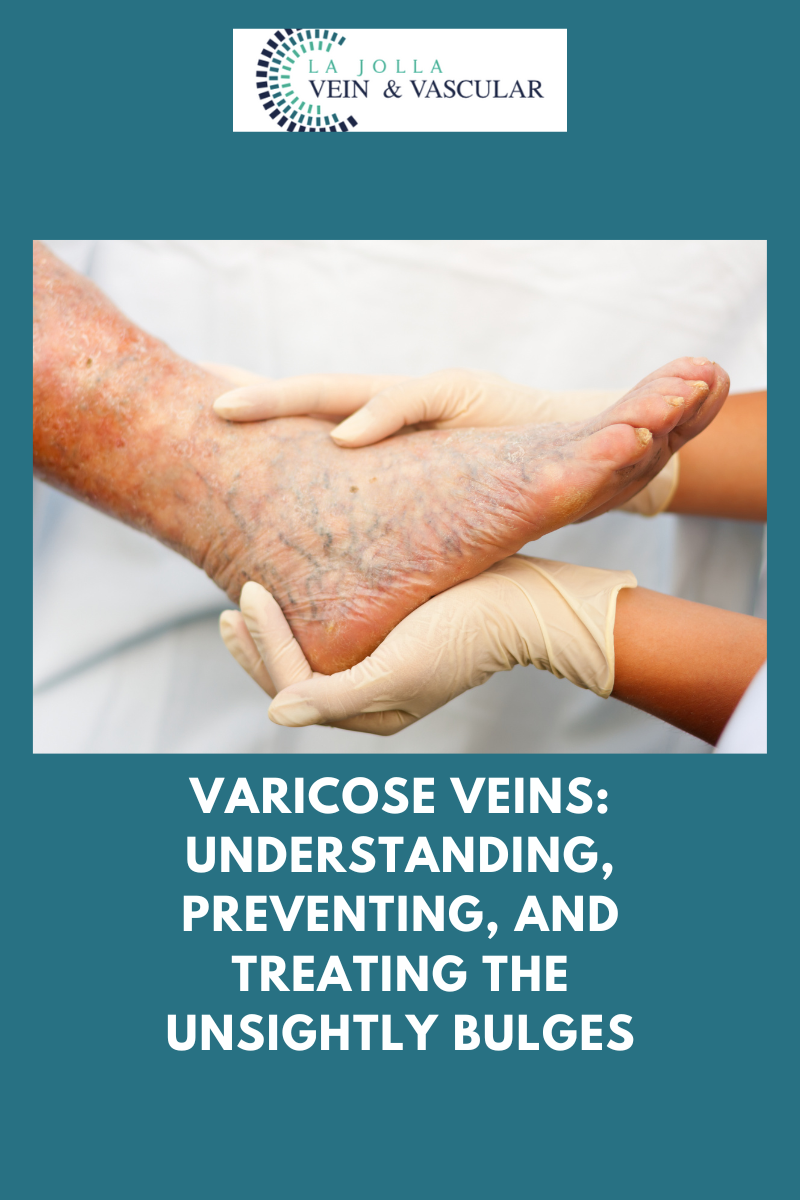
Sclerotherapy is a well-established and highly effective treatment for spider veins and reticular veins, particularly on the legs. The procedure involves the injection of a special medication directly into the affected veins. This powerful medication works its magic by causing the veins to collapse and gradually fade away.

Why Sclerotherapy?
You might wonder why sclerotherapy is the preferred choice for many vein specialists over alternatives like laser treatments. Here’s why:
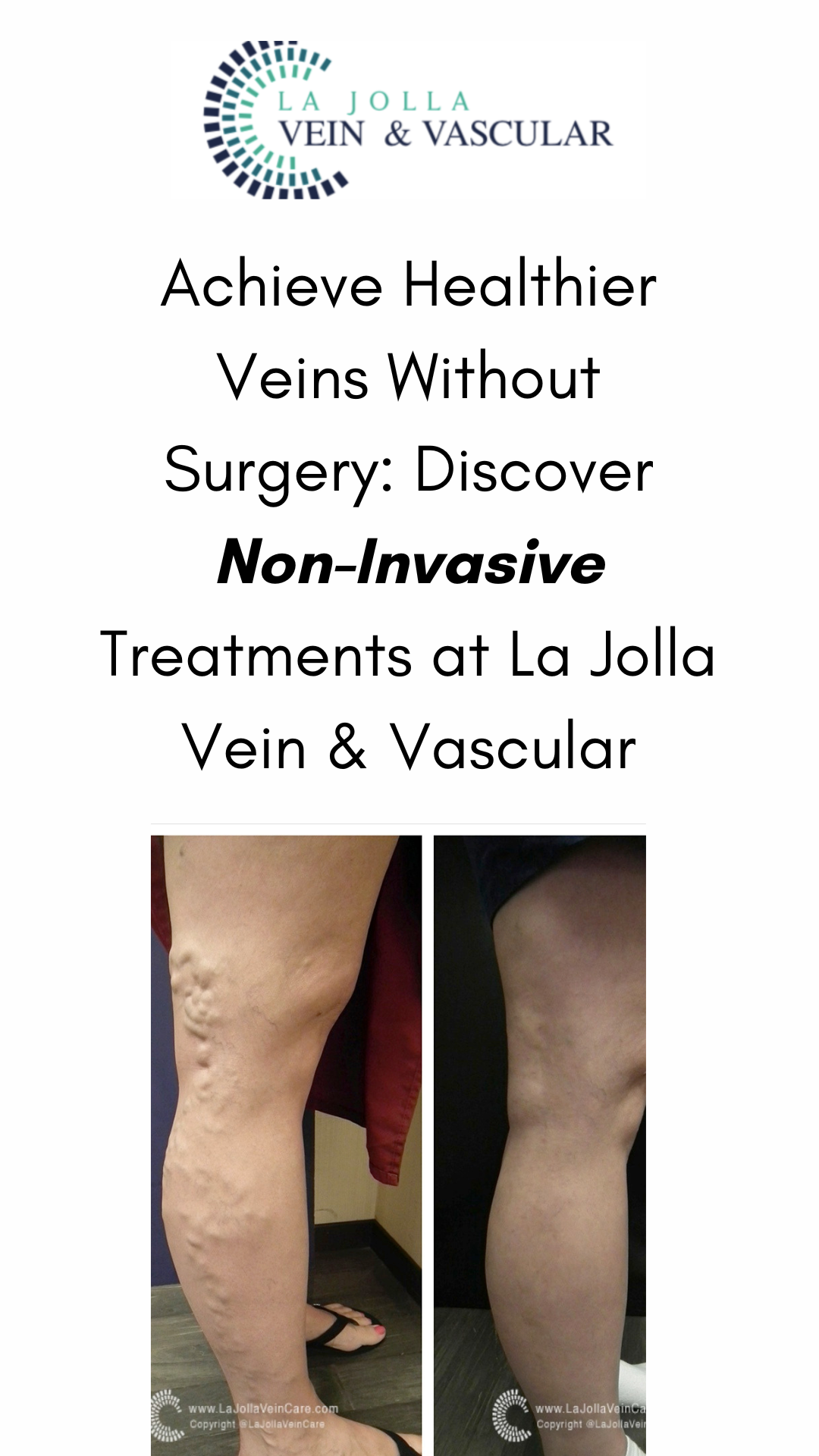
- Minimal Discomfort: Newer solutions like AscleraTM have made sclerotherapy more comfortable than ever. Patients can say goodbye to the pain associated with older saline solutions.
- Immediate Return to Activities: Unlike some treatments that require downtime, sclerotherapy allows you to resume your regular activities almost immediately after the procedure.
- Effective for Spider Veins: Sclerotherapy is particularly effective for spider veins, which often have underlying ‘feeder veins.’ These feeder veins can be easily treated with sclerotherapy but are not addressed by laser treatments.
What to Expect During Sclerotherapy Treatment
If you’re considering sclerotherapy, it’s natural to wonder about the treatment process. Here’s a step-by-step breakdown of what you can expect on your treatment days:
- Consent and Preparation: You’ll begin by signing a consent form. Afterward, you’ll change into shorts provided by the office to ensure easy access to the treatment area.
- Skin Cleaning: The treatment area will be thoroughly cleaned with alcohol to minimize the risk of infection.
- Injection: Using a fine needle, the sclerosant medication will be skillfully injected into your veins. This medication is the secret sauce that will work its wonders on your spider veins.
- Compression Stockings: After the procedure, you’ll be helped into compression stockings. These stockings play a vital role in improving the results of sclerotherapy.
- Walk It Off: To encourage optimal circulation, you’ll be advised to walk for 30 minutes before getting into your car. This simple step can make a significant difference in the treatment’s success.
Sclerotherapy is the magic wand that can make your spider veins disappear and restore your confidence in your legs’ beauty. With minimal discomfort, immediate results, and a straightforward procedure, it’s no wonder that sclerotherapy is a preferred choice for vein specialists. So, if you’re ready to say goodbye to spider veins, sclerotherapy might just be the enchanting solution you’ve been looking for.
“Bringing Experts Together for Unparalleled Vein and Vascular Care”
At La Jolla Vein & Vascular (formerly La Jolla Vein Care), we’re dedicated to providing expert vein and vascular care. Our specialists—Dr. Nisha Bunke, Dr. Sarah Lucas, and Dr. Amanda Steinberger—combine their extensive experience to offer you world-class treatment.
Our center is not only accredited but also recognized nationally as a teaching site and center of excellence.
If you’d like more information about our treatments or to schedule a consultation, call us at 858-550-0330.
Want to learn more about vein and vascular health? Check out our YouTube channel and visit our website at ljvascular.com.
For tips on varicose veins and treating venous insufficiency, follow us on Instagram and TikTok for fun and educational videos.
Explore more in-depth content on our blog, where we share useful insights and updates on vascular health.