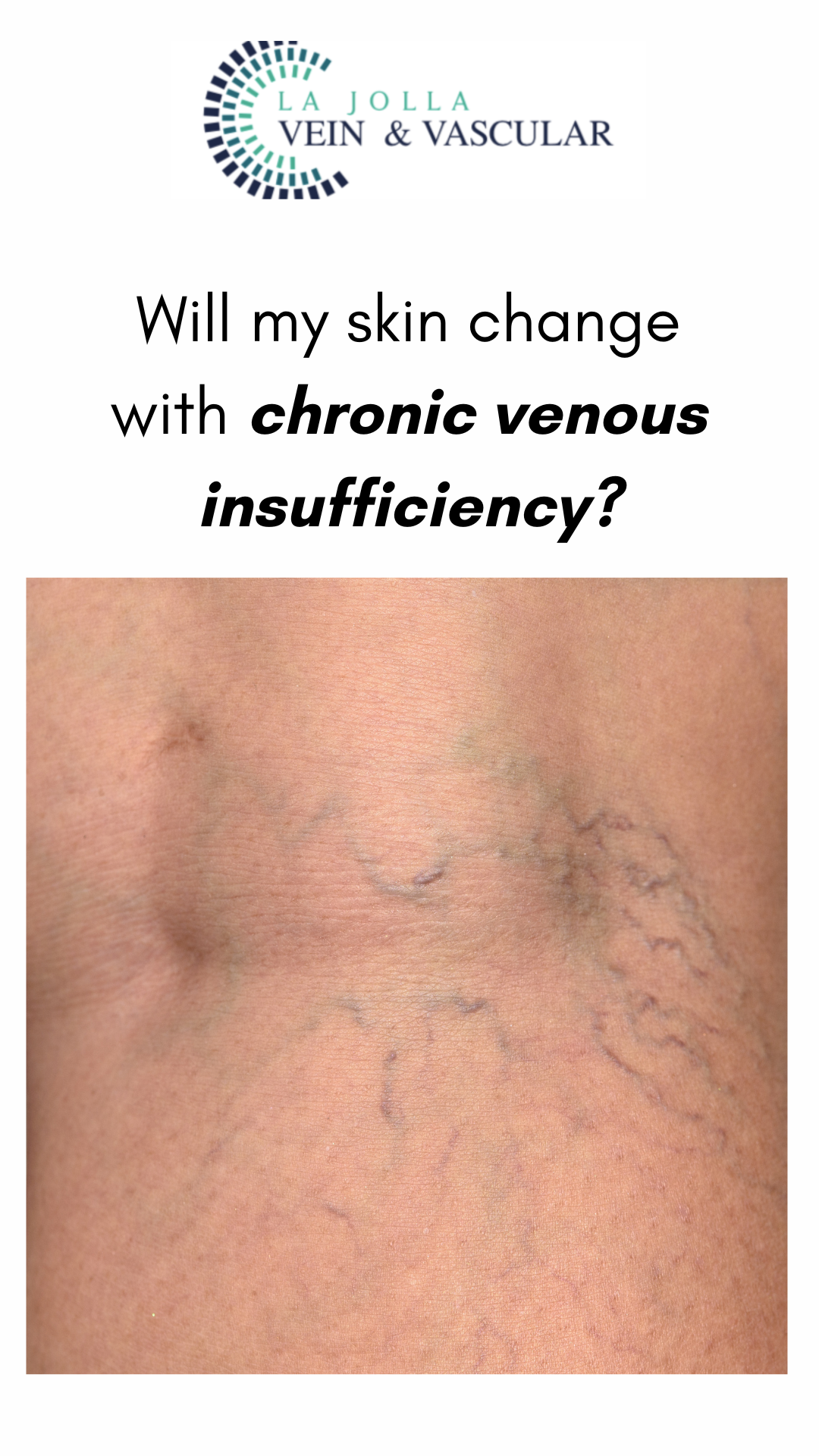
How Can I Expect My Legs to Appear Post-Spider Vein Treatment?
LJVascular2024-05-14T01:32:59-07:00What are spider veins?
Spider veins are the fine, thread-like reddish veins at the surface of the skin. These veins are not healthy. Veins are often considered a cosmetic issue, but they can be associated with underlying feeder veins, not visible to the naked eye. Feeder veins are the ‘blue veins’ also […]





![What do I need to know about venous disease? 11 What Do I Need to Know About Venous Disease? [2024]](https://ljvascular.com/wp-content/uploads/2024/03/Bunke-March-Blog-Thumbnail-37.png)

