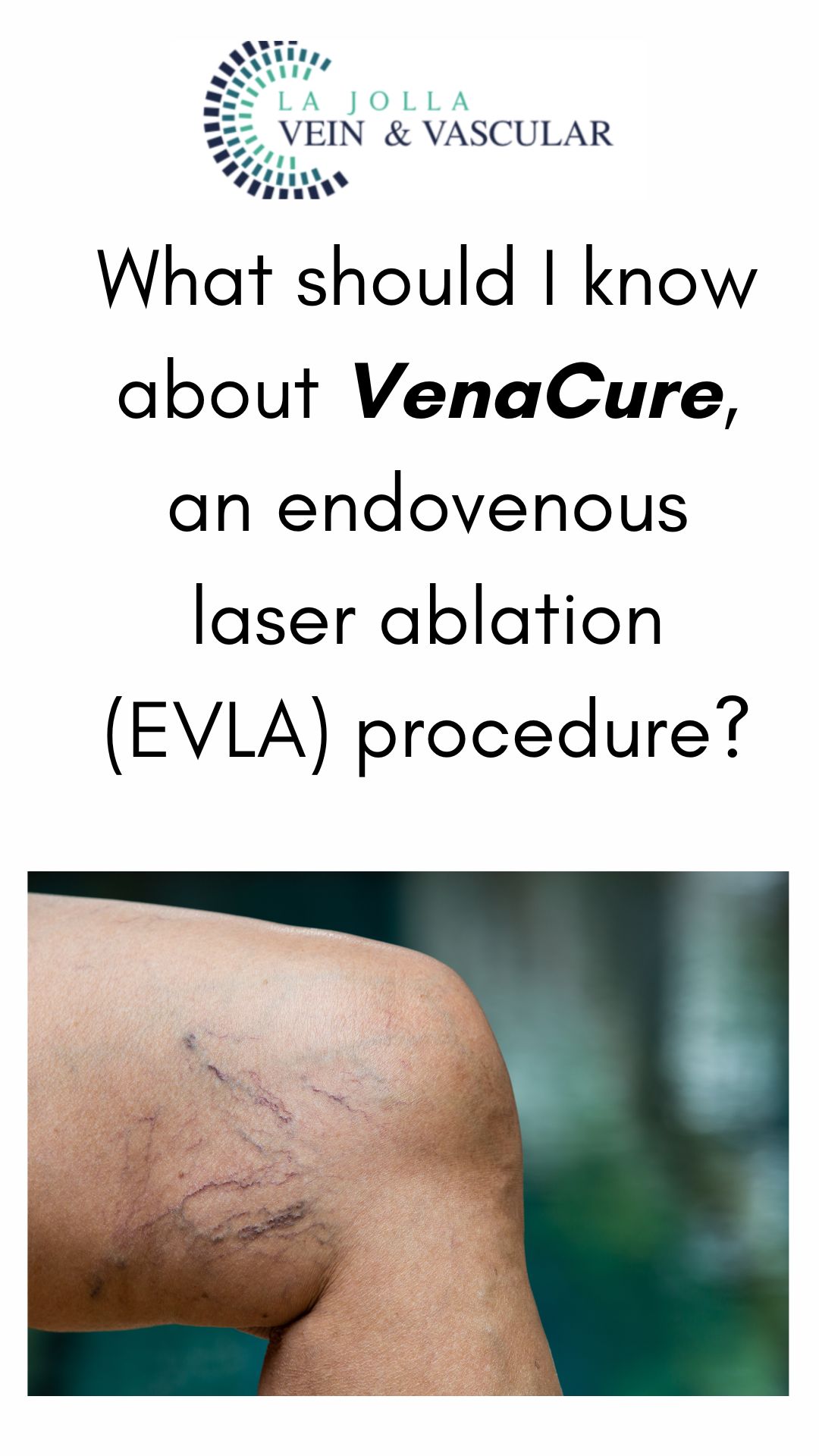
What should I know about VenaCure, an endovenous laser ablation (EVLA) procedure?
LJVascular2024-05-13T23:46:48-07:00VenaCure, an endovenous laser ablation (EVLA) procedure, offers a cutting-edge solution for addressing backward flow, or “reflux,” in the saphenous veins. These veins, comprising the great and small saphenous veins, are pivotal superficial veins running along the inner and back of the leg, respectively. By targeting reflux in these veins, VenaCure provides […]