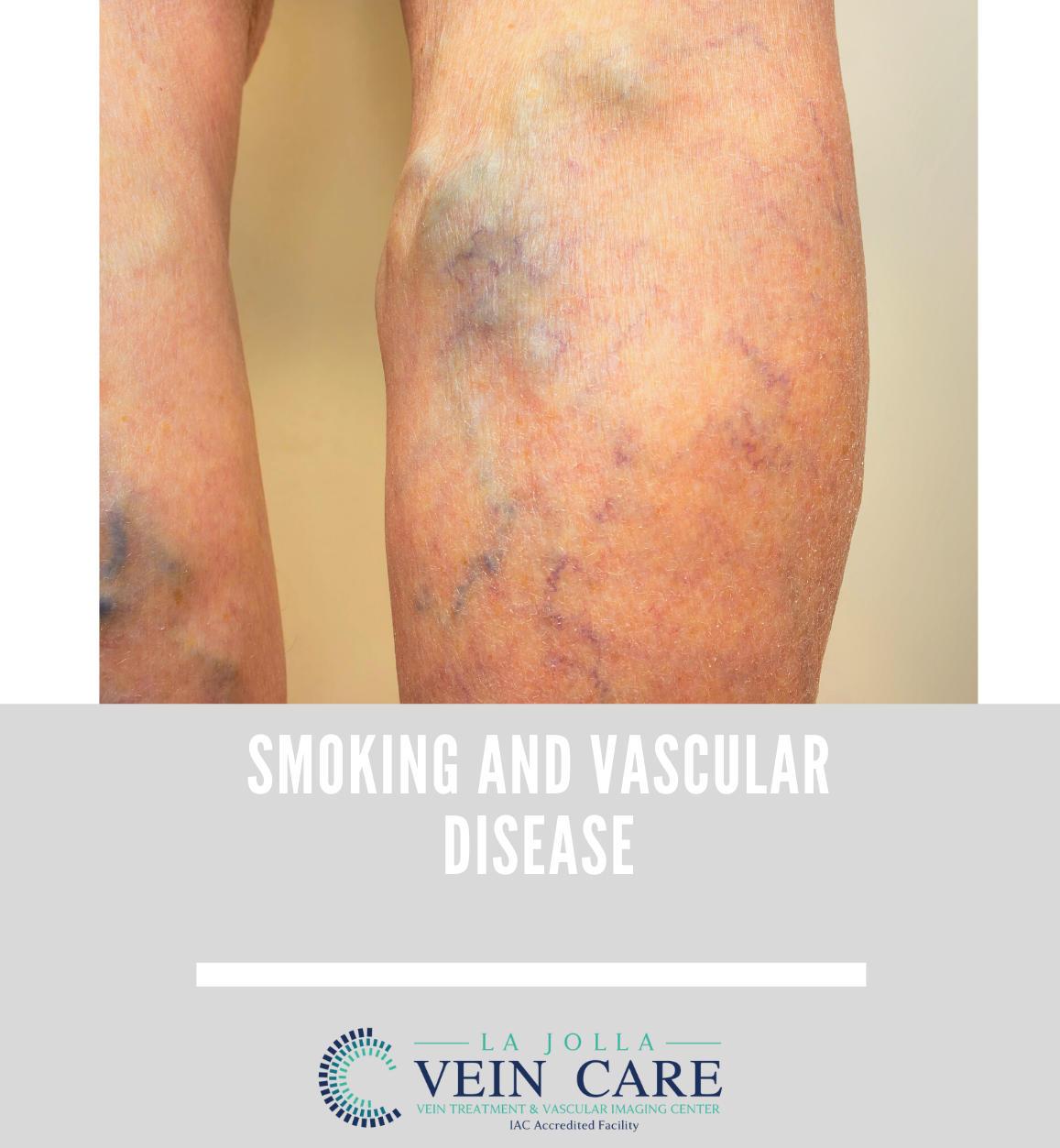
Smoking and Vascular Disease
LJVascular2022-04-04T14:53:33-07:00Smoking and Vascular Disease
The reality of cigarettes is that it is not one product. Every time you smoke, you not only ingest nicotine, but hundreds of other deadly chemicals in the tobacco leaf, paper, contaminants and fertilizers used to grow tobacco. Over time the accumulation of these products causes serious harm to multiple […]