DVT Unveiled: Deep Vein Thrombosis
LJVascular2024-10-24T20:16:52-07:00DVT Unveiled: Deep Vein Thrombosis
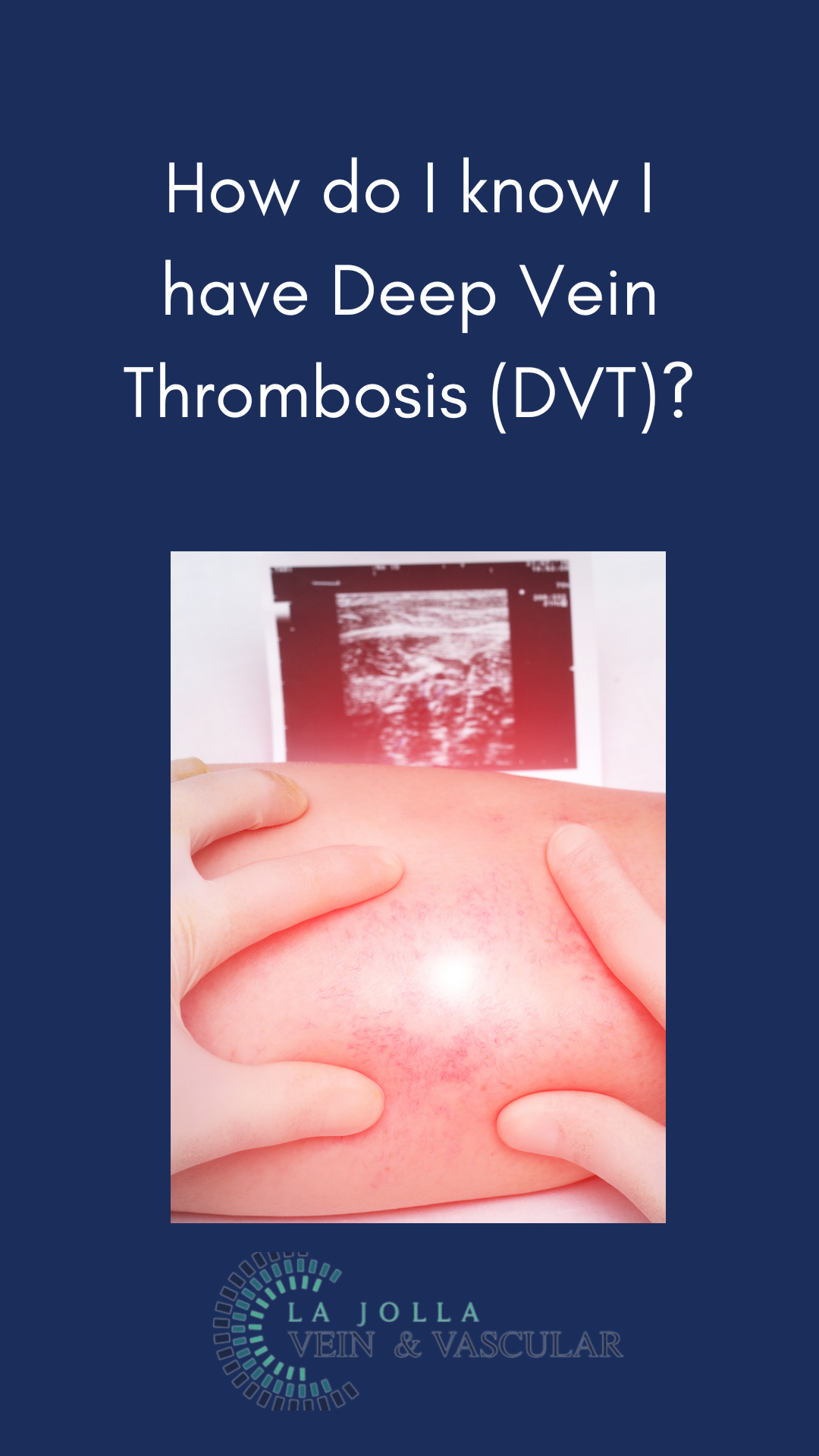
Deep Vein Thrombosis (DVT) may not always be visible on the surface, but its potential consequences are far from hidden. In this blog post, we’ll explore what DVT is, why it’s a serious medical condition, how it can be diagnosed, and the importance of vigilance in its detection.
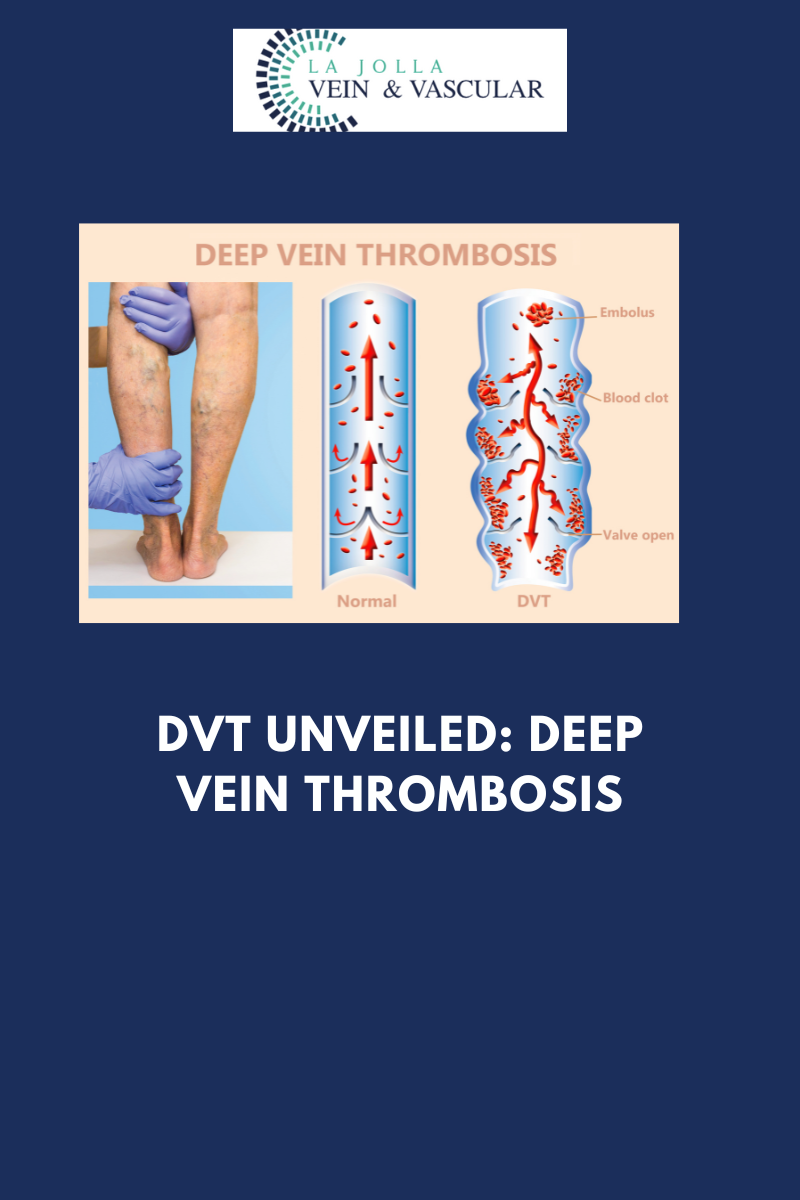
Understanding Deep Vein Thrombosis (DVT) or What is Deep Vein Thrombosis (DVT)?
Deep Vein Thrombosis, often referred to as DVT, is a condition characterized by the formation of a blood clot within the deep veins of the legs. While it may begin as a seemingly innocuous clot, the risk lies in its ability to travel through the bloodstream and reach the lungs, causing a potentially life-threatening pulmonary embolism.
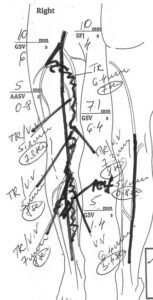
The Diagnostic Power of Duplex Ultrasound
Diagnosing DVT is a critical step in preventing its dangerous consequences. This is where Duplex ultrasound, a valuable diagnostic tool, comes into play. Here’s how it works:
- Experienced Vascular Sonographer: A trained vascular sonographer is a key player in diagnosing DVT. Their expertise ensures accurate and reliable results.
- Duplex Ultrasound Examination: Duplex ultrasound combines traditional ultrasound (B-mode) with Doppler ultrasound, allowing healthcare providers to visualize blood flow and detect clots within the deep veins.
- Indications for DVT Study: A DVT study is typically performed when an individual presents with signs and symptoms of lower extremity DVT. These symptoms may include leg pain and swelling, often accompanied by redness and warmth.
- Routine Screening: In certain situations, such as after a vein procedure or other surgical interventions, routine DVT screening may be performed as a preventive measure to identify clots before they cause harm.
Preparing for the DVT Study
Fortunately, preparing for a DVT study is straightforward and requires no special steps. Here’s what you should know:
- No Special Preparation: Unlike some medical tests that require fasting or specific preparations, a DVT study typically does not necessitate any special preparation.
Vigilance Beyond the Legs: Upper Extremity Venous Study
While DVT is most commonly associated with the lower extremities, it’s essential to recognize that blood clots can develop elsewhere in the body. This includes the upper arms and neck. An Upper Extremity Venous Study is a diagnostic ultrasound of the upper arms and neck, performed when a person experiences signs and symptoms such as pain and swelling in the arms.
Deep Vein Thrombosis is a serious medical condition with the potential for life-threatening consequences. Timely diagnosis through Duplex ultrasound is essential for effective intervention and prevention of complications like pulmonary embolism.
If you or someone you know experiences symptoms such as leg pain, swelling, or unexplained discomfort, seeking prompt medical attention and considering a DVT study is crucial. Vigilance and early detection can be life-saving when it comes to this hidden danger lurking within our veins.
Our Commitment to Vein and Vascular Care
“Bringing Experts Together for Unparalleled Vein and Vascular Care”
La Jolla Vein & Vascular (formerly La Jolla Vein Care) is committed to bringing experts together for unparalleled vein and vascular care.
Nisha Bunke, MD, Sarah Lucas, MD, and Amanda Steinberger, MD are specialists who combine their experience and expertise to offer world-class vascular care.
Our accredited center is also a nationally known teaching site and center of excellence.
For more information on treatments and to book a consultation, please give our office a call at 858-550-0330.
For a deeper dive into vein and vascular care, please check out our Youtube Channel at this link, and our website https://ljvascular.com
For more information on varicose veins and eliminating underlying venous insufficiency,
Please follow our social media Instagram Profile and Tik Tok Profile for more fun videos and educational information.
For more blogs and educational content, please check out our clinic’s blog posts!