La Jolla’s excellent ultrasound tech team
LJVascular2023-10-11T17:37:19-07:00La Jolla’s excellent ultrasound tech team
In the realm of vascular health, nothing less than precision and accuracy will suffice. Venous ultrasound tests, which stand as integral tools for diagnosing vascular conditions, necessitate the involvement of adept and highly trained professionals. In this blog post, allow us to introduce you to the often unsung heroes who toil behind the scenes—the Registered Vascular Technologists (RVTs). These dedicated individuals conduct venous ultrasound tests with unwavering commitment, upholding the most stringent standards of quality and accuracy.
Deconstructing the Role of a Registered Vascular Technologist (RVT)
Venous ultrasound tests are far from conventional medical imaging procedures. They demand a unique skill set and a profound comprehension of vascular anatomy and functionality. This is where RVTs come to the forefront. But who exactly are these RVTs, and what distinguishes them from the rest?
Embarking on a Journey with the Experts: RVTs
- Specialized Education: RVTs embark on a journey of rigorous training to excel in their field. This voyage begins with the completion of a comprehensive two-year ultrasound program, serving as the foundational building block of their expertise. Yet, it’s vital to note that their learning journey does not culminate here.
- Additional Clinical Training: Beyond the confines of the classroom, RVTs partake in extensive clinical training. This hands-on experience allows them to bridge the gap between theoretical knowledge and its real-world application. Through this process, they fine-tune their skills, ensuring proficiency.
- Certification by ARDMS: The American Registry for Diagnostic Medical Sonography® (ARDMS®) stands as the gold standard for sonographers. RVTs are individuals who have successfully met ARDMS’s stringent certification requirements. This painstaking process guarantees that RVTs remain at the vanguard of their profession, consistently upholding the highest standards of competence.
The Indispensable Role of RVTs in Venous Ultrasound Testing
Venous ultrasound testing represents a complex and intricate procedure, necessitating precision and adherence to precise protocols. Here’s why the involvement of an RVT in the testing process holds utmost significance:
- Adherence to Accreditation Standards: Accredited ultrasound facilities must adhere to stringent standards to preserve their accreditation. RVTs, as consummate professionals, rigorously follow specific protocols for each study, ensuring that the results meet these exacting accreditation standards and are marked by the highest quality.
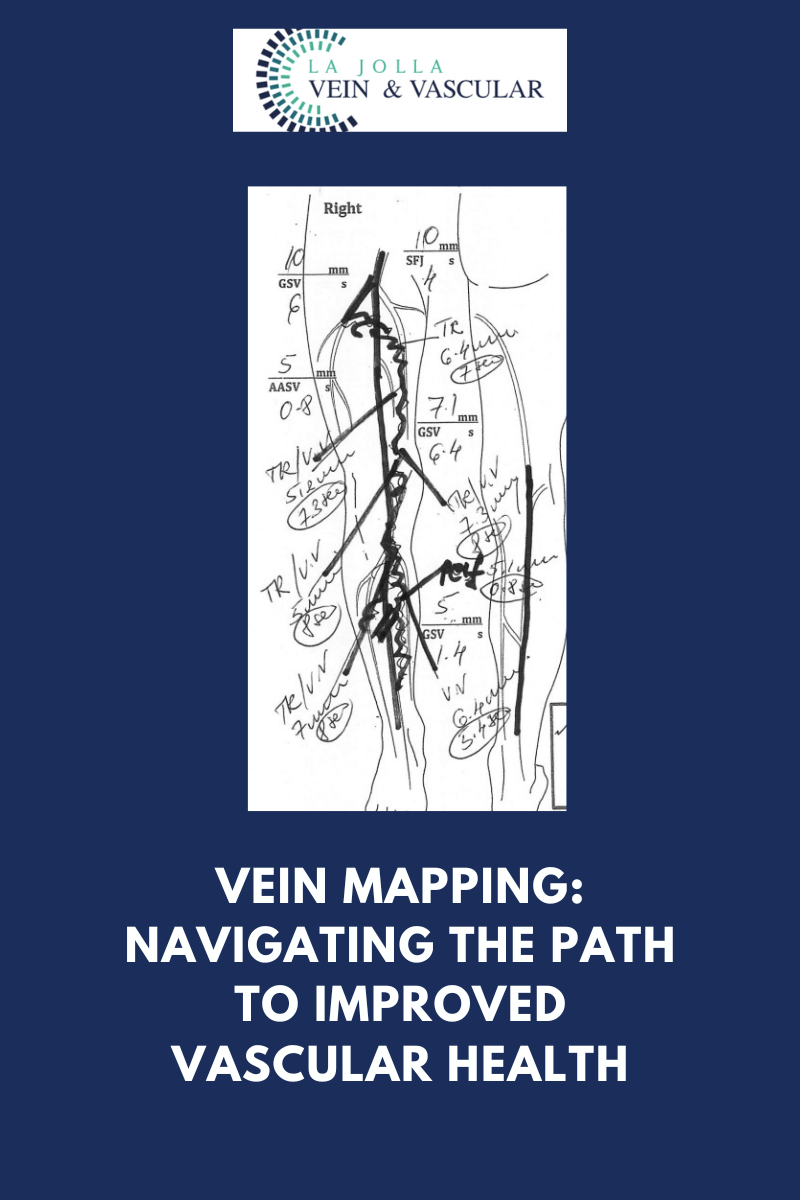
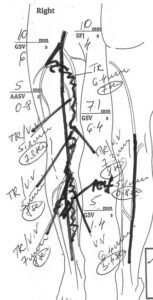
- Anatomic Expertise: RVTs possess an intricate knowledge of vascular anatomy. They exhibit a keen awareness of precisely where to capture images and how to utilize special waveforms, ensuring the accurate visualization of blood flow.
- Collaboration with Physicians: Every image that an RVT captures undergoes a meticulous review by physicians. This symbiotic collaboration guarantees that the findings are not only precise but also guides the formulation of the most effective course of action for patients.
The unwavering dedication and consummate expertise of Registered Vascular Technologists (RVTs) underpin the accuracy of venous ultrasound testing. These highly trained professionals assume a pivotal role in your journey toward optimal vascular health, guaranteeing that each test is executed with precision and aligns with the loftiest standards.
The next time you find yourself in the midst of a venous ultrasound test, take solace in the knowledge that your well-being is entrusted to the capable hands of an RVT. Their unswerving commitment to excellence and their contribution to accurate diagnoses constitute indispensable facets of your overarching state of health.
“Bringing Experts Together for Unparalleled Vein and Vascular Care”
La Jolla Vein & Vascular (formerly La Jolla Vein Care) is committed to bringing experts together for unparalleled vein and vascular care.
Nisha Bunke, MD, Sarah Lucas, MD, and Amanda Steinberger, MD are specialists who combine their experience and expertise to offer world-class vascular care.
Our accredited center is also a nationally known teaching site and center of excellence.
For more information on treatments and to book a consultation, please give our office a call at 858-550-0330.
For a deeper dive into vein and vascular care, please check out our Youtube Channel at this link, and our website https://ljvascular.com
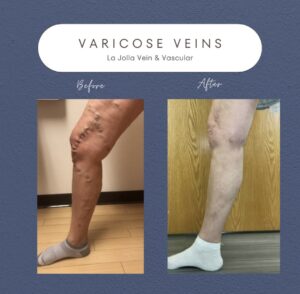
For more information on varicose veins and eliminating underlying venous insufficiency,
Please follow our social media Instagram Profile and Tik Tok Profile for more fun videos and educational information.
For more blogs and educational content, please check out our clinic’s blog posts!