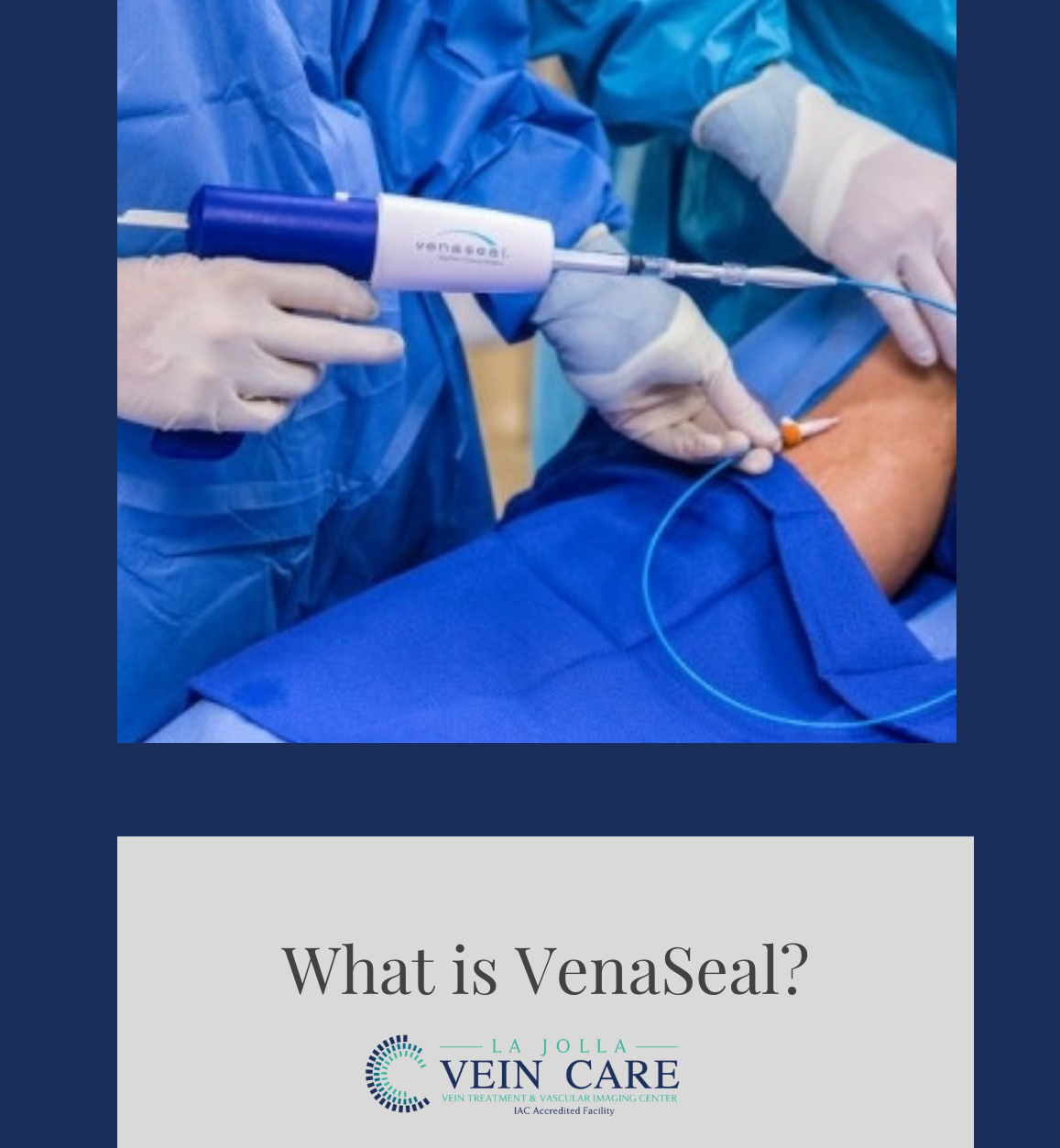
What is VenaSeal?
LJVascular2022-04-15T11:21:27-07:00The U.S. Food and Drug Administration (FDA) approved the VenaSeal Closure System to permanently treat varicose veins by sealing the affected superficial veins using an adhesive agent.
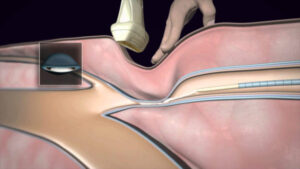
The VenaSeal Closure System is a unique, minimally invasive treatment that uses a safe-for-the-body medical glue to quickly and […]