What could be causing your varicose veins?
LJVascular2022-12-13T14:16:03-08:00What are varicose veins?
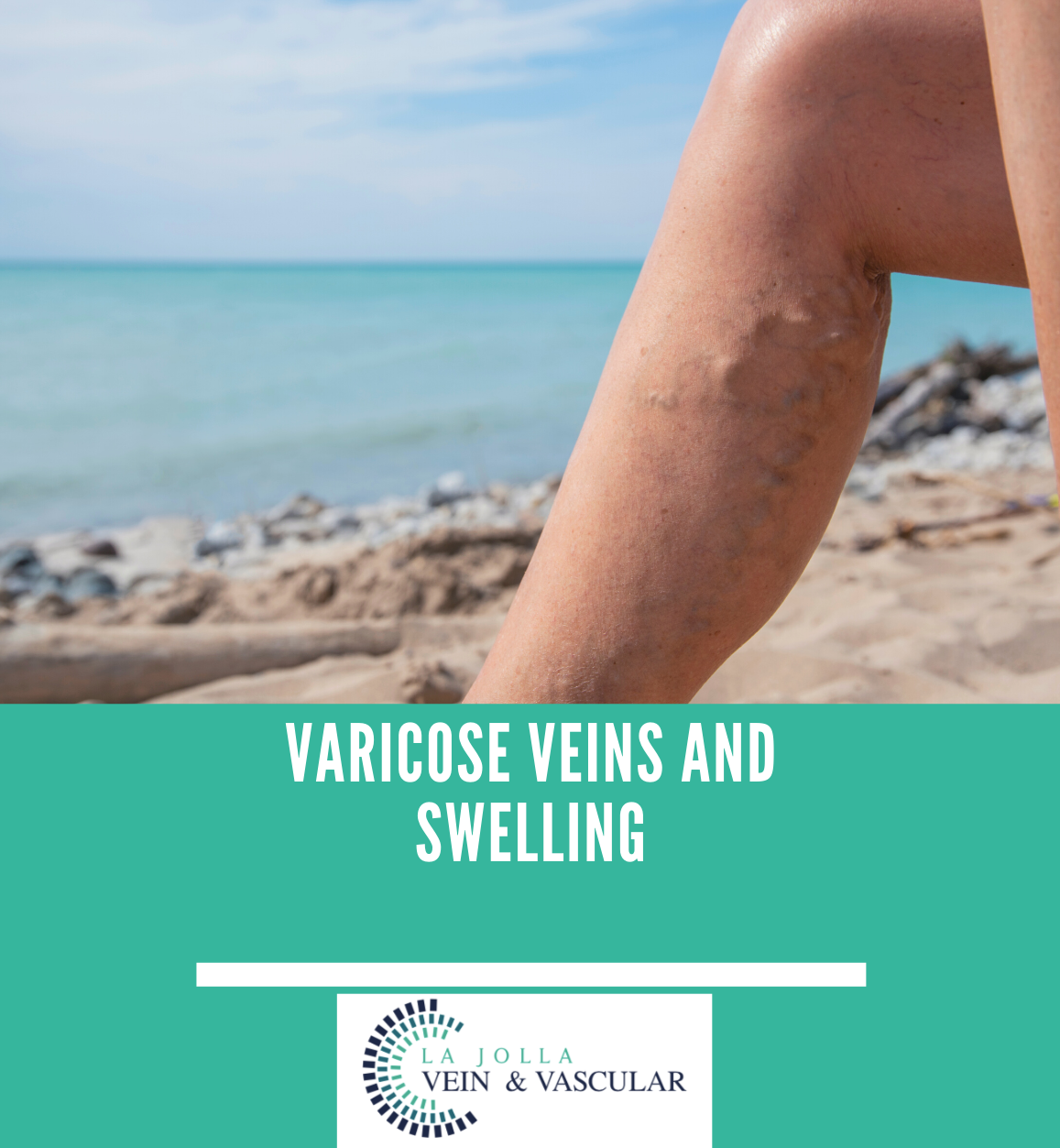
Varicose veins are the twisted, bulging veins just beneath the surface of the skin. Varicose veins are swollen, twisted veins that you can see just under the surface of the skin. These veins usually occur in the legs, but they also can form in other parts of the […]