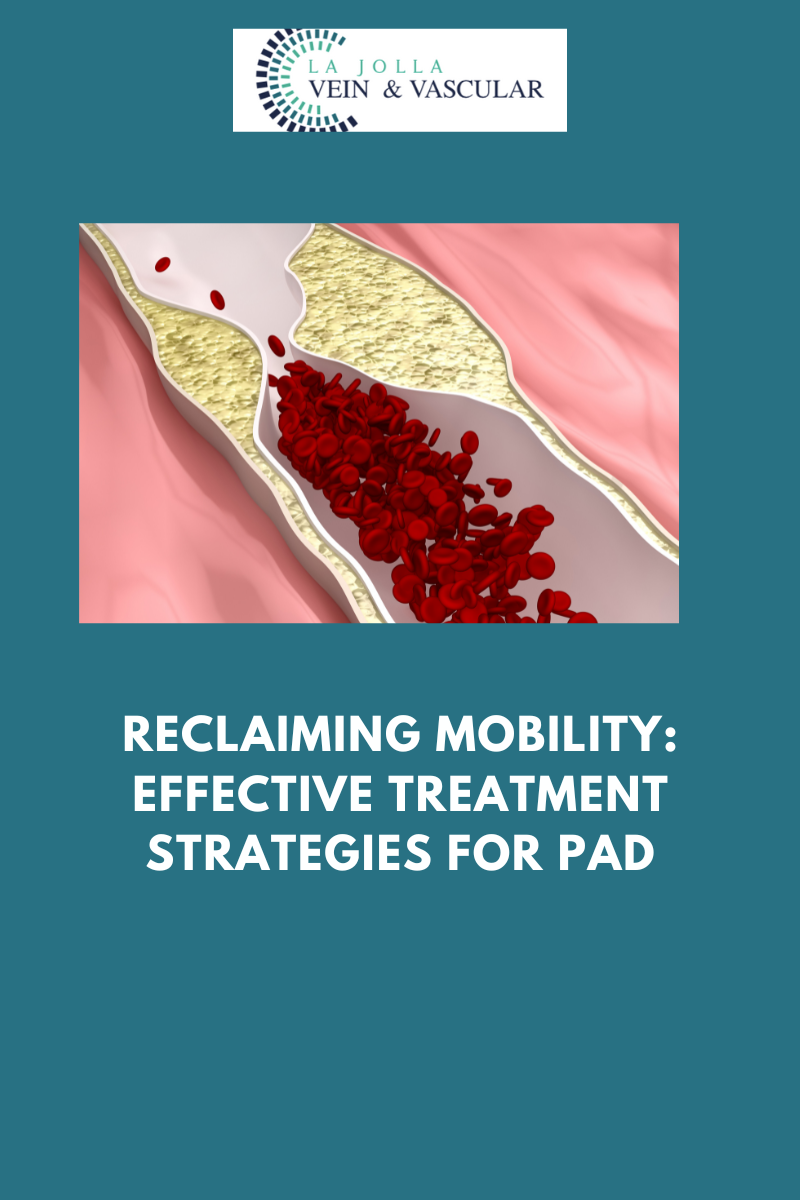
Reclaiming mobility: effective treatment strategies for PAD
LJVascular2024-10-28T01:17:37-07:00Reclaiming Mobility: Effective Treatment Strategies for PAD
Peripheral Arterial Disease (PAD) can be a challenging condition, but with the right approach to treatment, you can regain control of your life. The goals of PAD treatment are to manage symptoms, such as leg pain, and halt the progression of atherosclerosis, which […]






![What do I need to know about venous disease? 8 What Do I Need to Know About Venous Disease? [2024]](https://ljvascular.com/wp-content/uploads/2024/03/Bunke-March-Blog-Thumbnail-37.png)