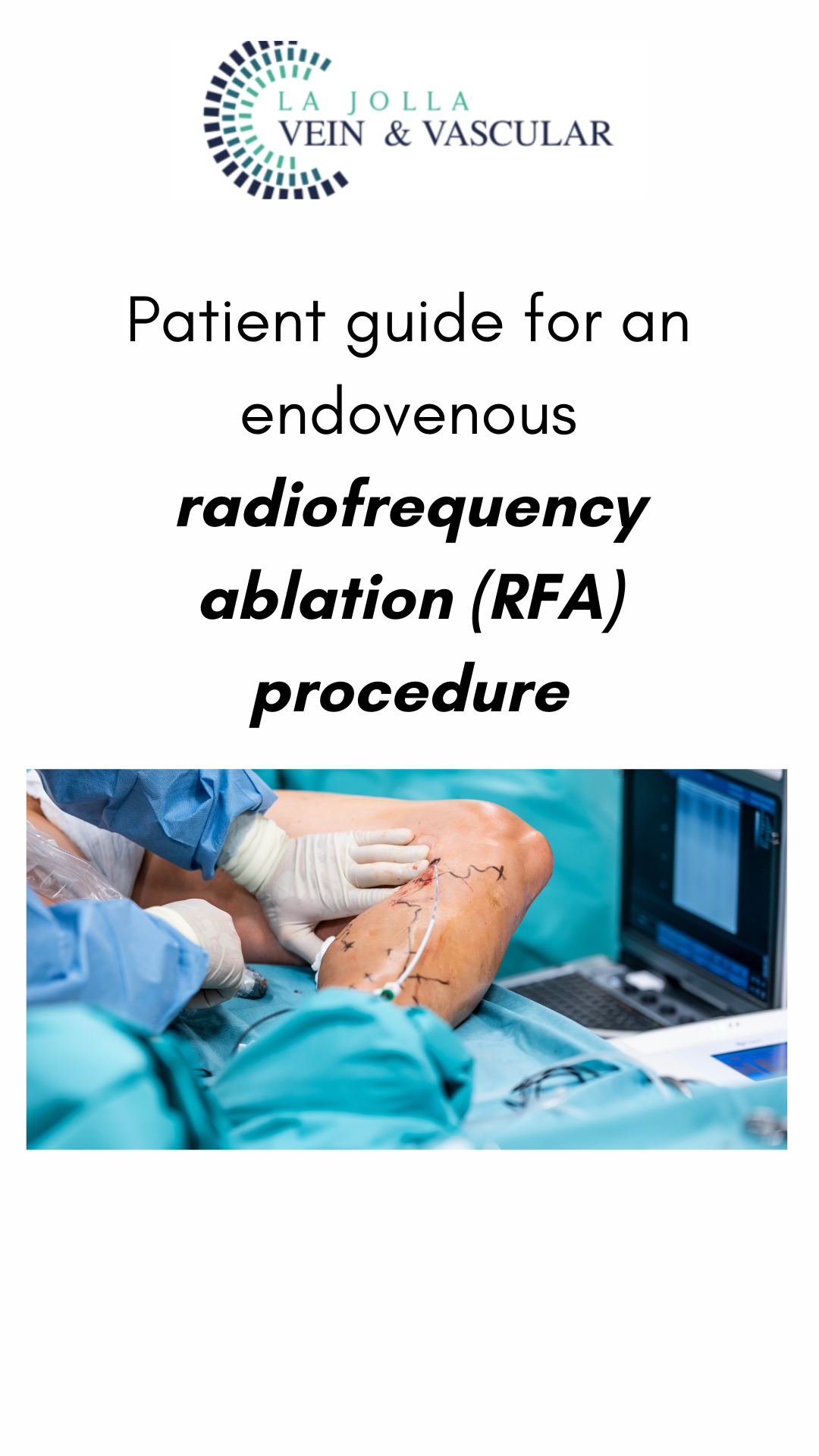
Patient guide for an endovenous radiofrequency ablation (RFA) procedure
LJVascular2024-05-14T01:22:46-07:00ClosureFast™, an endovenous radiofrequency ablation (RFA) procedure, offers a revolutionary solution for combating the backward flow of blood, known as “Venous reflux,” in the saphenous veins. These veins, namely the great saphenous veins and small saphenous veins, are pivotal superficial veins located along the inner and back of the leg, respectively.