Self Care 101 for Varicose Veins
Conservative Management and Self-Care for Varicose Veins
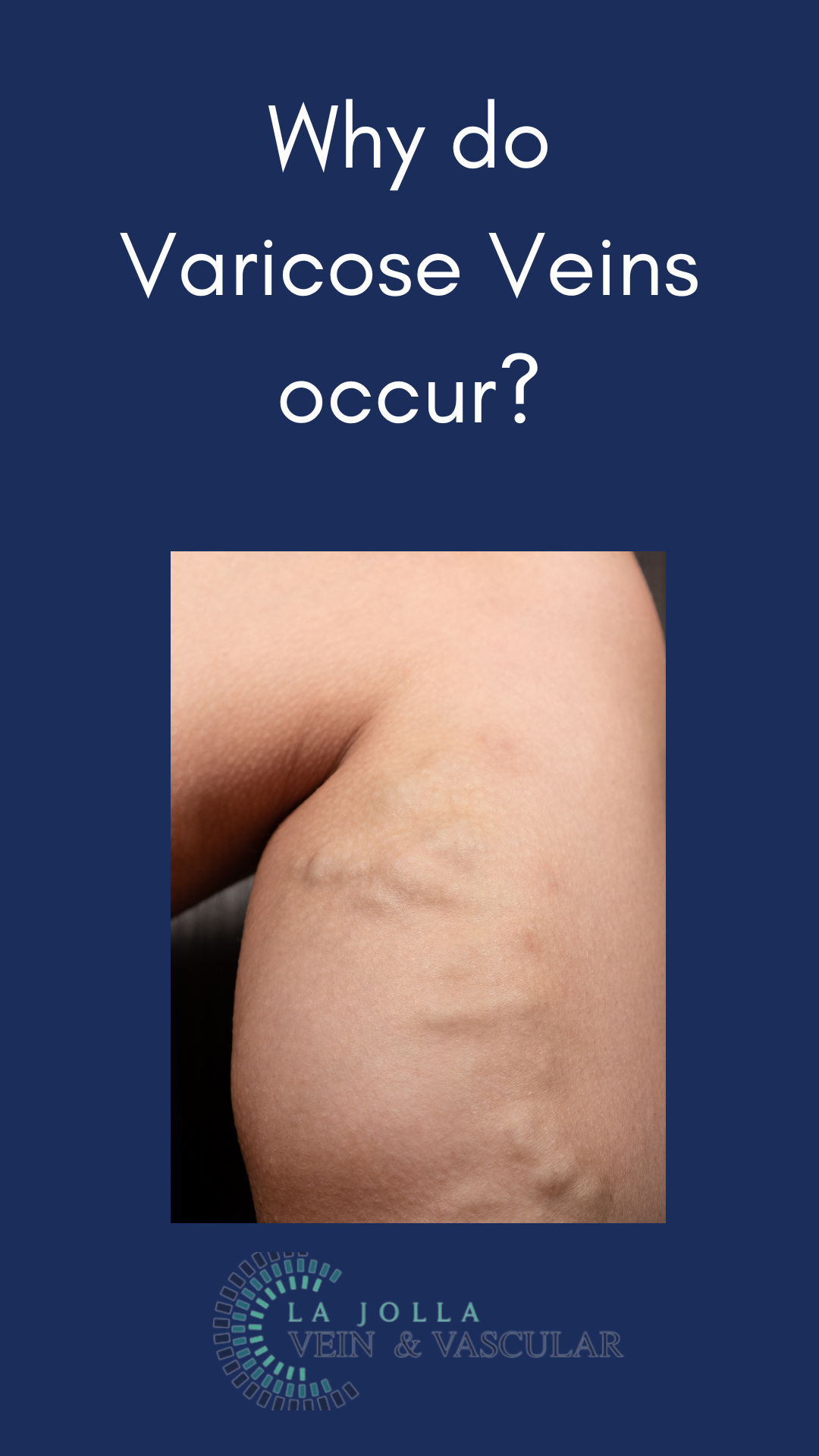
Varicose veins can cause discomfort and lead to complications such as thrombophlebitis (blood clots within veins) and vein rupture. While conservative management and lifestyle changes can’t make varicose veins disappear, they can ease symptoms and help reduce the risk of complications. These measures are especially helpful for individuals who are not candidates for vein procedures or wish to delay interventional treatments.
Compression Stockings
One of the most effective conservative treatments for varicose veins is wearing compression stockings. These elastic stockings apply pressure to the veins, aiding in blood circulation and preventing blood from flowing backward and pooling in the legs. It’s important to use graduated, medical-grade compression stockings for maximum benefit, as regular TED hose are not sufficient for active patients with venous disease.
Compression stockings come in different strengths, with 20-30 mmHg being the most common for treating varicose veins. Your doctor can recommend the appropriate strength for your condition. It’s also worth noting that in patients with peripheral arterial disease (PAD), diabetes, or neuropathies, compression may be contraindicated or a lesser strength may be advised.
Avoiding Inactivity
Prolonged periods of standing or sitting can worsen varicose vein symptoms. To keep blood moving during these times, try the following tips:
- At Work: Take walking breaks and incorporate walking into your lunch hour.
- While Sitting: Flex your feet up and down 10 times an hour.
- While Standing: Raise yourself up and down on your toes or rock back and forth on your heels.
These simple activities can help improve circulation and alleviate some of the discomfort associated with varicose veins.
Exercise and Varicose Veins
Regular exercise can significantly benefit individuals with varicose veins. Engaging in activities such as walking, swimming, and cycling promotes blood circulation and helps reduce symptoms. Avoid high-impact exercises that put excessive strain on your legs, as they might worsen the condition.
Dietary Supplements
Certain dietary supplements can help manage the symptoms of venous disease. For example, horse chestnut and grape seed extract are known to be beneficial. Vasculera, a prescription medication, may also be helpful for some individuals. However, it’s crucial to consult with your primary care physician before starting any new supplements or medications, as they may have side effects or interact with other medications.
Heat Management
Heat can exacerbate symptoms of leg pain and varicose veins. During hot weather or while using heat sources like hot baths or saunas, be mindful of your condition and take steps to keep your legs cool to prevent worsening symptoms.
Conclusion
While conservative management won’t eliminate varicose veins, these strategies can help ease symptoms and prevent complications. Compression stockings, staying active, regular exercise, and the careful use of dietary supplements can all contribute to better vein health. Always consult with your healthcare provider to develop a personalized plan that’s right for you. If you’re not a candidate for vein procedures or prefer to delay them, these self-care measures can make a significant difference in managing your varicose veins.
“Bringing Experts Together for Unparalleled Vein and Vascular Care”
La Jolla Vein & Vascular (formerly La Jolla Vein Care) is committed to bringing experts together for unparalleled vein and vascular care.
Nisha Bunke, MD, Sarah Lucas, MD, and Amanda Steinberger, MD are specialists who combine their experience and expertise to offer world-class vascular care.
Our accredited center is also a nationally known teaching site and center of excellence.
For more information on treatments and to book a consultation, please give our office a call at 858-550-0330.
For a deeper dive into vein and vascular care, please check out our Youtube Channel at this link, and our website https://ljvascular.com
For more information on varicose veins and eliminating underlying venous insufficiency,
Please follow our social media Instagram Profile for more fun videos and educational information.
For more blogs and educational content, please check out our clinic’s blog posts!