How To Make Varicose Veins Vanish Without Surgery
Physicians have many options for treating varicose veins. The choice often depends on the severity and cause of the problem. It’s important that patients are carefully evaluated so treatment can be tailored to individual needs.
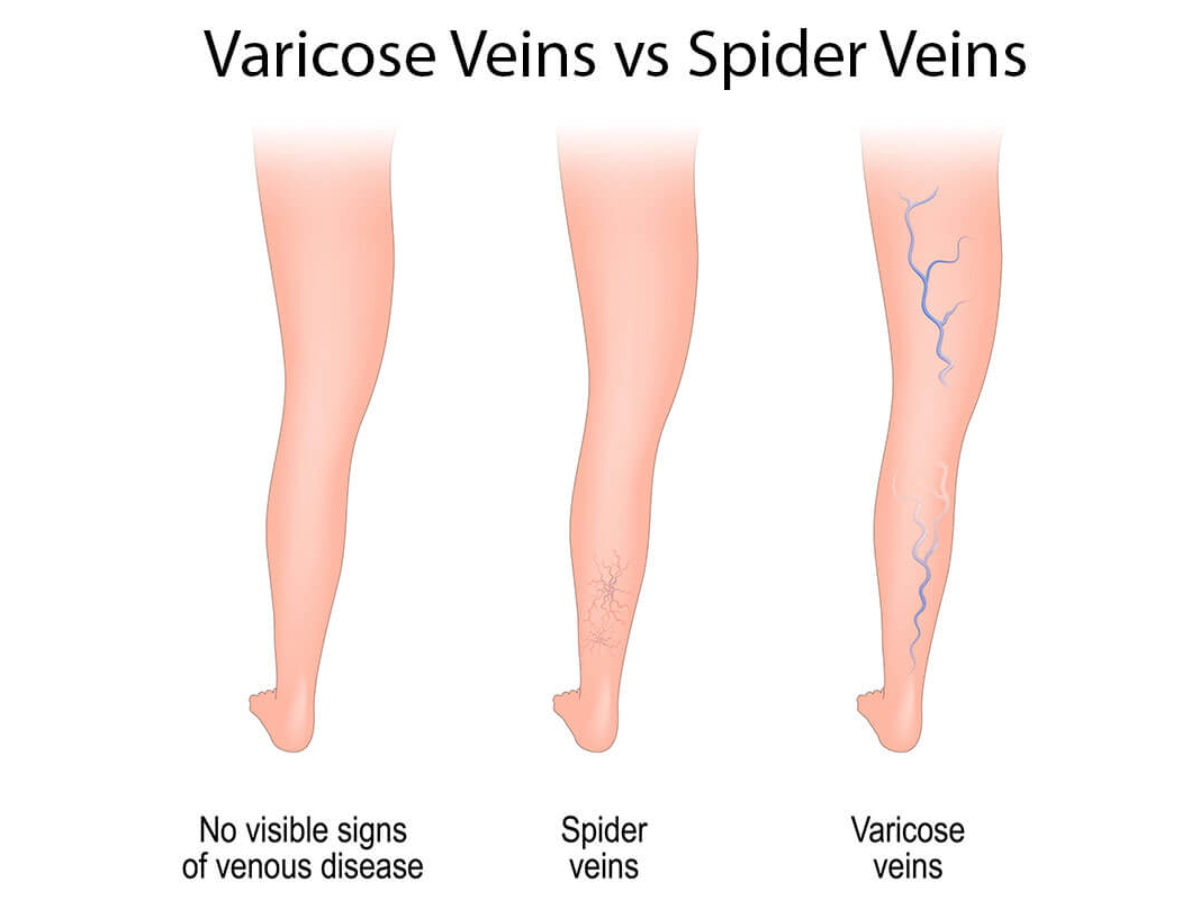
In some cases, varicose veins may present a primarily cosmetic problem. In others, they may be a symptom of a more severe underlying circulatory condition that should be addressed by a vascular specialist.
Compression hosiery can be used to provide support and reduce varicose veins symptoms such as the aching and tiredness associated with but they cannot make varicose veins disappear. There are no supplements or creams that can make varicose veins disappear. There are a variety of creams, lotions, and ointments that are advertised in newspapers and magazines to make veins disappear. There is no scientific evidence that these creams or lotions can make varicose and spider veins disappear. Once veins are dysfunctional, it is a mechanical problem and the valves cannot be repaired. But, they can be removed. There are many ways to accomplish this.
Sclerotherapy is used for smaller varicose veins and for spider veins, also known as telangiectasia. A fine needle is used to inject a chemical solution into the veins. The chemical causes the vein to collapse and eventually disappear. The procedure can be done in a doctor’s office and doesn’t require an anesthetic. Patients feel only a slight burning when the chemical is injected. Often several sessions are needed to treat the veins.
Foam sclerotherapy or ultrasound-guided foam sclerotherapy is used to treat large varicose veins.
Ambulatory Phlebectomy is an alternative to foam sclerotherapy, and involves making a series of tiny incisions along the length of the vein and gently removing the vein in sections using a hook. The procedure can be done on an outpatient basis and can be used for both large and small veins.
Radiofrequency ablation is a minimally invasive procedure involving using a catheter to introduce an electrode into the saphenous vein (great, small, or accessory saphenous veins). The energy from the electrode shrinks and seals off the vein. Nearby healthy veins take over the job of carrying blood from the legs.
Surgical ligation and stripping are rarely performed because the newer, minimally invasive procedures have replaced surgery for removing varicose veins.
For more information about treatment types and non-surgical methods to make varicose veins vanish, go to www.july01ljvascular.com.

Before and After Pictures: Varicose Vein Treatment at La Jolla Vein Care. At La Jolla Vein Care, we utilize minimally invasive techniques to make varicose veins vanish- all without open surgery or general anesthesia.