Dr. Fronek Featured in National Vein Magazine
Web@ljvascular.com2021-11-04T15:42:23-07:00Past ACP President and La Jolla Vein Care’s Dr. Helane Fronek, MD, FACPh, FACP was featured in this summer’s Vein Magazine. The 5-page interview with Dr. Fronek discusses topics such as her career and perspectives in the fields of venous disease and medicine. She is described as:
‘Professionally, Dr. Froenk sees patients at La Jolla Vein Care, educates medical students as an assistant clinical professor at the UC San Diego School of Medicien, is the author of the Fundamentals of Phlebology, is a past President of the American College of Phlebology (ACP), is the first recipient of the ACP’s Leadership Award and is recognized as an Honorary Memeber of the organization……..she is also a blogger on The Huffington Post and has recently added Life Coach to her distinguished resume…’
Past ACP President and La Jolla Vein Care’s Dr. Helane Fronek, MD, FACPh, FACP was featured in this summer’s Vein Magazine. The 5-page interview with Dr. Fronek discusses topics such as her career and perspectives in the fields of venous disease and medicine.
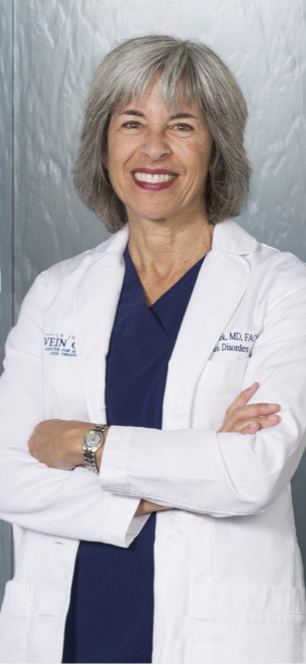
Dr. Helane Fronek, MD, FACPh, FACP is a Past ACP President, author of the Fundamentals of Phlebology, Assistant Clinical Professor at UCSD School of Medicine and presently sees patients at La Jolla Vein Care, located at the Scripps Memorial Campus.
La Jolla Vein Care is grateful to have such a talented doctor on our staff. You can read Dr. Fronek’s blog at helanefronekmd.wordpress.com.