Patient Reviews and Testimonials
LJVascular2023-01-14T13:09:42-08:00La Jolla Vein & Vascular is a state-of-the-art medical center dedicated exclusively to the diagnosis and treatment of venous conditions and arterial conditions.
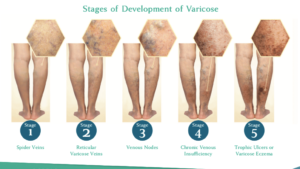
Venous conditions include varicose veins, spider veins, and venous leg ulcers, chronic venous insufficiency, edema, lymphedema, and deep vein thrombosis. Arterial conditions and treatments such as peripheral arterial disease […]