Diving Deeper into Deep Vein Thrombosis
LJVascular2024-10-21T21:35:39-07:00Diving Deeper into Deep Vein Thrombosis (DVT)
Deep Vein Thrombosis (DVT) is a medical condition that arises when blood clots develop within the deep veins of the legs, thighs, or pelvis. To navigate the complexities of DVT, it’s vital to comprehend its causes, symptoms, and the potential dangers it poses. In this enlightening blog post, we embark on a journey to unravel the mechanics behind blood clot formation, explore the risks associated with DVT, and delve into the spectrum of treatment options available for managing this condition.
Demystifying the Genesis of Blood Clots
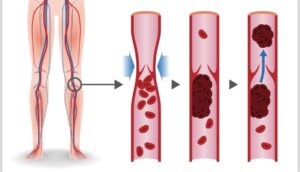
Blood clots within the veins, such as those characteristic of DVT, come to fruition due to the malfunctioning of valves residing within the venous system. These valves bear the pivotal responsibility of ensuring the smooth flow of blood back to the heart. However, when these valves weaken or falter, the harmonious circulation of blood becomes compromised, ushering in the formation of clots. While DVT predominantly occurs within the deep veins of the lower extremities, it can also manifest in other regions of the body, encompassing the upper limbs.
The Intricacies of the Circulatory System and Blood Clot Formation
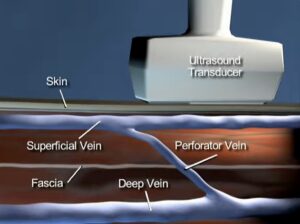
The human circulatory system comprises two essential components: arteries and veins. Arteries dutifully ferry oxygen-rich blood away from the heart, and their robust, muscular walls can withstand the forceful pumping action of the heart. In contrast, veins, lacking such muscular linings, rely on the rhythmic contractions of nearby muscles to propel blood towards the heart.
Unraveling the Mechanisms of Blood Clot Development
The venous system within the legs is a dynamic network encompassing two principal types of veins: superficial and deep. The journey of blood from superficial veins to deep veins is facilitated by perforator veins, aided by a system of one-way valves. When the pace of blood flow slows down or blood pools within the veins, platelets can aggregate, setting the stage for the formation of a blood clot, scientifically referred to as a thrombus. While a blood clot within the deep venous system is not inherently perilous, it can take a life-threatening turn if it becomes dislodged and embarks on a journey to the pulmonary vein, resulting in a pulmonary embolism.
Spotlight on Symptoms and Risks Associated with DVT
Timely identification of the symptoms of DVT holds the key to prompt intervention:
- Leg Pain During Walking: Experiencing muscle cramps or sharp pain while walking.
- Sharp Calf Pain in the Affected Limb: Sudden and intense discomfort in the calf.
- Red or Discolored Skin on the Affected Limb: Changes in skin color.
- Swelling in the Affected Area: Notable enlargement of the limb.
- Sudden Onset Leg Swelling: Abrupt and significant leg swelling.
- Enlarged Veins: Prominent veins becoming apparent.
- Increased Warmth in the Swollen Area: Heightened temperature in the affected region.
If a blood clot detaches and embarks on a journey to the lungs, it can culminate in a pulmonary embolism, characterized by:
- Sudden Breathlessness or Shallow Breathing: Difficulty in breathing.
- Rapid Breathing: Accelerated respiratory rate.
- Elevated Heart Rate: Increased pulse rate.
- Chest Pain Exacerbated by Deep Breathing: Discomfort in the chest intensified by deep breaths.
Treatment Avenues for DVT
A multitude of treatment options are at the disposal of healthcare professionals for effectively managing DVT:
- Blood Thinners: These anticoagulant medications thwart the enlargement and detachment of clots. Common examples encompass injectable medications such as enoxaparin (Lovenox) and oral medications like Eliquis, Xarelto, and Pradaxa.
- Clot Busters: Thrombolytic drugs come into play for severe DVT or Pulmonary Embolism (PE) cases where other treatments prove ineffective. These drugs can dissolve blood clots but may carry a risk of bleeding.
- Filters: In scenarios where blood thinners are contraindicated, a vena cava filter can be inserted to prevent dislodged clots from reaching the lungs.
- Compression Stockings: These specialized knee-high socks play a pivotal role in mitigating blood pooling and the formation of clots in the legs.
Deep Vein Thrombosis is a sobering medical condition that demands prompt attention and treatment. By unraveling the mechanisms underlying blood clot formation and recognizing the telltale symptoms, individuals can proactively seek medical assistance when needed, potentially thwarting life-threatening complications. An array of treatment avenues exists to manage DVT effectively, and consultation with a healthcare professional stands as an imperative step for receiving personalized care and guidance.
Read More Deep Vein Thrombosis:







![What do I need to know about venous disease? 17 What Do I Need to Know About Venous Disease? [2024]](https://ljvascular.com/wp-content/uploads/2024/03/Bunke-March-Blog-Thumbnail-37.png)
![What do I need to know about venous disease? 18 venous disease | What Do I Need to Know About Venous Disease? [2024]](https://ljvascular.com/wp-content/uploads/2024/03/2-1-300x300.png)