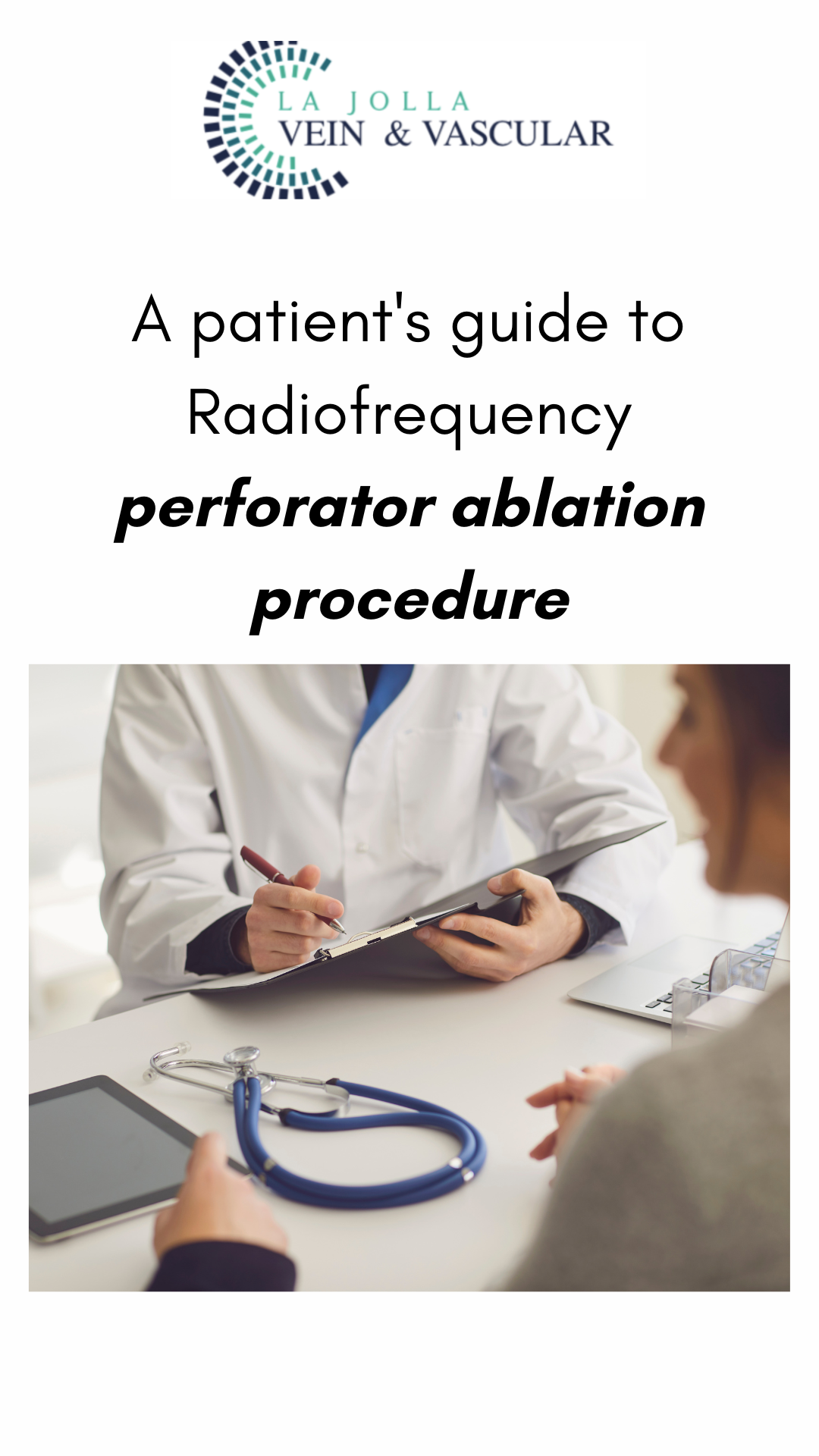
A patient’s guide to Radiofrequency perforator ablation procedure
LJVascular2024-05-13T23:29:31-07:00Radiofrequency perforator ablation emerges as a crucial procedure for addressing perforator veins, the short connections between deep and superficial veins. These veins, vital for maintaining proper circulation, can suffer from valve damage and retrograde blood flow, leading to various vein disorders and potential skin complications. Understanding the function of perforator veins and the […]



![What do I need to know about venous disease? 9 What Do I Need to Know About Venous Disease? [2024]](https://ljvascular.com/wp-content/uploads/2024/03/Bunke-March-Blog-Thumbnail-37.png)