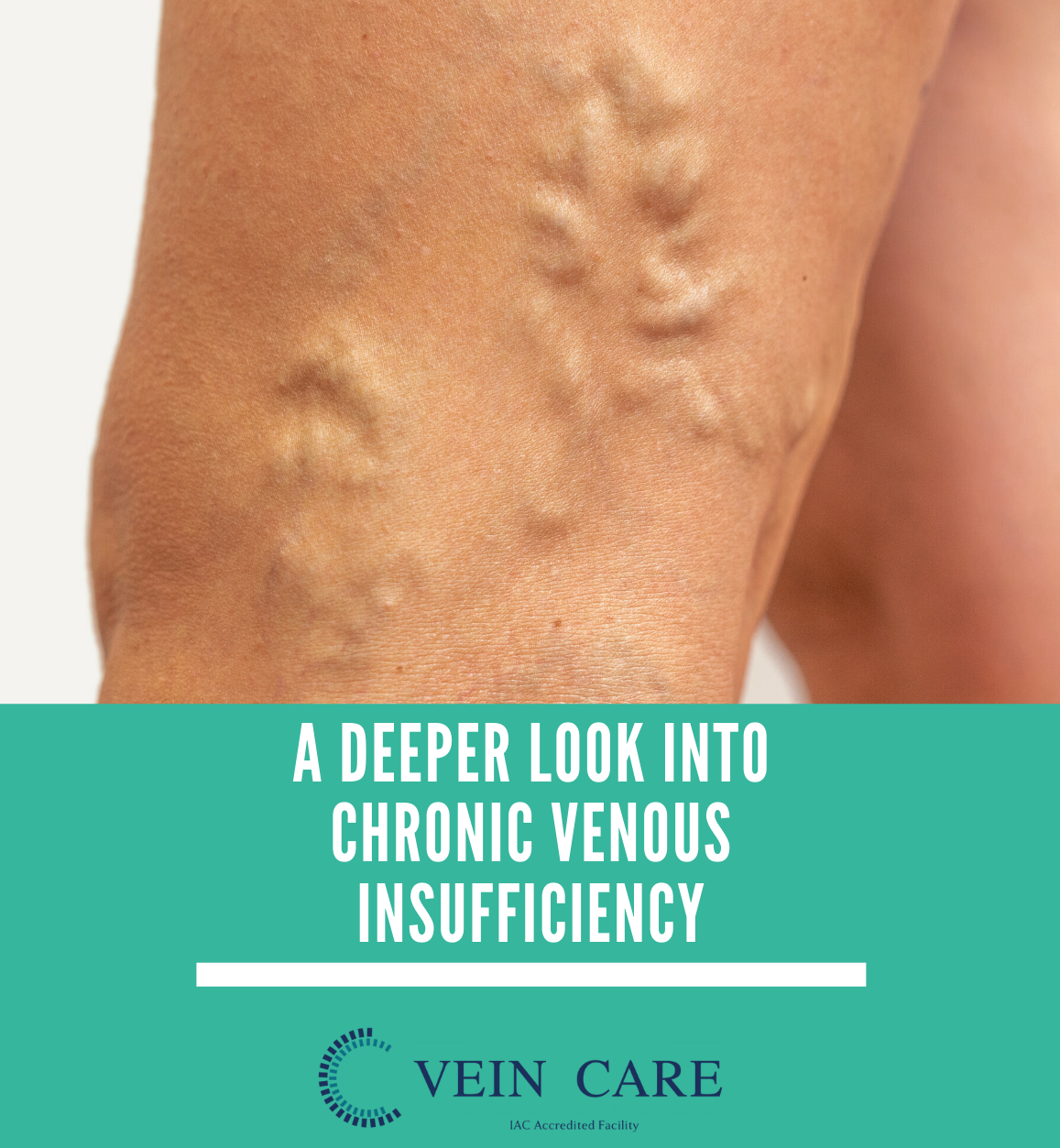
A deeper look into chronic venous insufficiency
LJVascular2022-04-15T15:36:06-07:00What is chronic venous insufficiency?
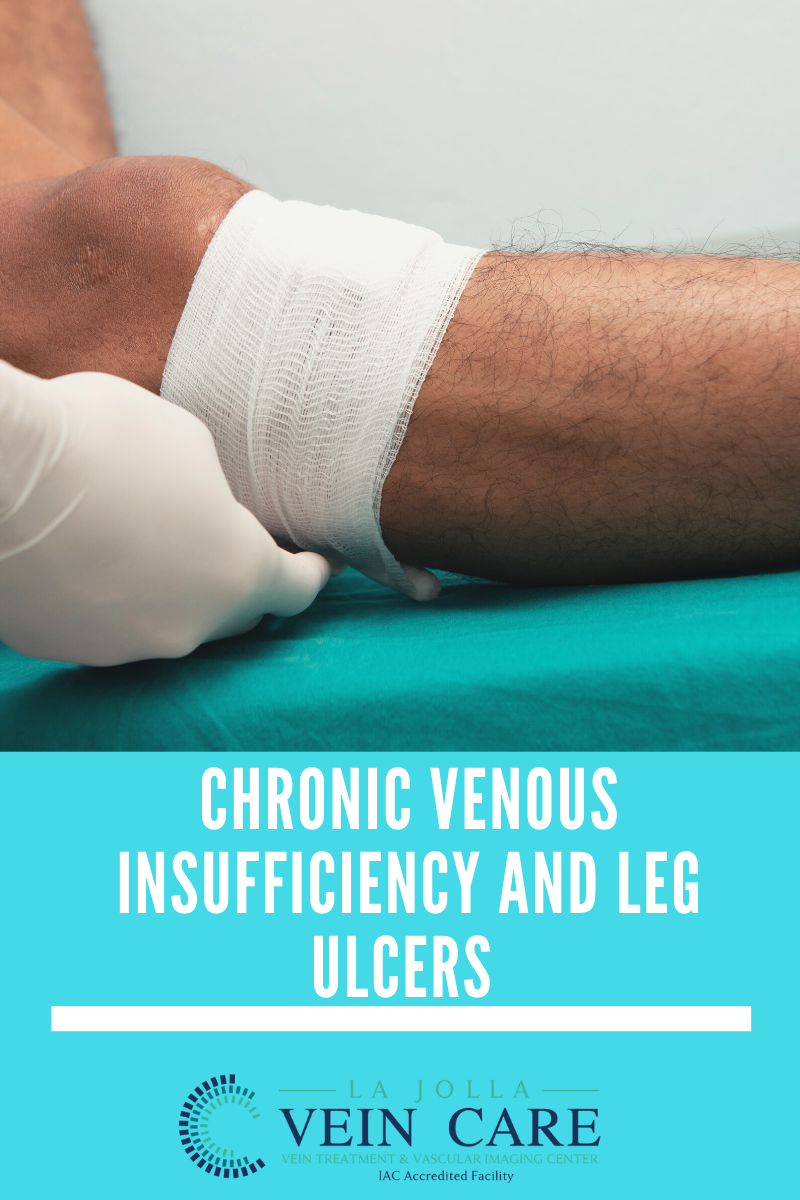
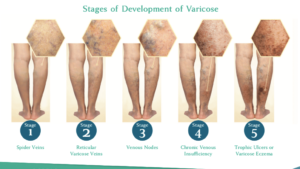
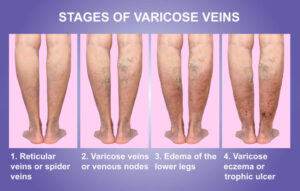
Chronic venous insufficiency (CVI) is an inflammatory condition caused by long standing, untreated venous reflux disease. Commonly, venous reflux disease causes a collection of symptoms such as leg swelling, heaviness, fatigue and varicose veins. But, over time, when blood is no longer circulating properly in the leg […]