What is VenaCure?
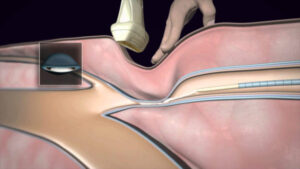
LJVascular2022-04-15T15:42:25-07:00VenaCure is an endovenous laser ablation (EVLA) procedure for backwards flow (or “reflux”) in your saphenous vein(s).
VenaCure Laser is also referred to as endovenous laser ablation therapy (EVLT). The great and small saphenous veins are the two main superficial veins of the leg. They run along the inner leg and the […]