Peripheral Arterial Disease – Diagnosis
At La Jolla Vein & Vascular, we have highly trained physicians who offer a comprehensive diagnosis to develop customized treatments of Peripheral artery disease (PAD). We understand that no two patients’ conditions are similar. Our full-service vascular lab provides state-of-the-art testing to ensure that our physicians address each patient case quickly and accurately. Our doctors and nurses also have broad experience in this field and use advanced tools to achieve limb-saving results even for challenging, impaired patients. Our PAD diagnosis procedure involves the following:
Detailed Physical Exam
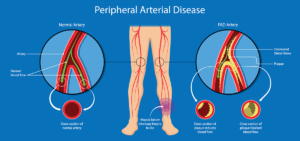
To help diagnose Peripheral Arterial Disease, our skilled doctor will start by doing a thorough physical examination. The doctor will also want to learn about your signs, symptoms, personal health history, risk factors, and family health history. The doctor will ask you several questions regarding your medical conditions, such as diabetes, heart disease, and kidney disease. They will also ask you whether you experience pain or cramps in your leg while walking or exercising.
The doctor will also ask about your family history of PAD and other heart diseases. You will also discuss your smoking habit, either current or in the past. After gathering the information, the doctor will proceed to perform a detailed physical examination. The process involves checking for weak pulses in your leg, listening for poor blood flow in the legs using a stethoscope. The physician will also check for any problems on your legs, such as sores, swelling, and pale skin.
Detailed Physical Exam
Ankle-brachial index (ABI)
Ankle-brachial index (ABI test) helps diagnose PAD. This test usually compares the blood pressure in your arm with the blood pressure in your ankle. The doctor usually uses a pressure cuff together with an ultrasound device. Sometimes, the physician may request you to walk on a treadmill and have the doctor take the readings before and immediately after the exercise. The procedure will help the doctor to capture the severity of the narrowed arteries.
Arterial Ultrasound
La Jolla Vein & Vascular doctors also use ultrasound-guided procedures to determine whether a specific vein or artery is blocked or open. The procedure is non-invasive, meaning that you will not experience any pain. The technique visualizes the artery with sound waves that measure the blood volume that flows in the veins and arteries. After the procedure, the patients receive a thorough consultation. The doctor will recommend the most effective treatment option to help promote blood flow to the feet and leg.
The treatment will help reduce leg pain, promote healing of sores and increase the mobility of the affected limb. Doctors utilize two main ultrasound methods. The first method is the Doppler ultrasound utilized to locate areas with blockages or reduced blood flow. The procedure involves using a handheld device that sends sound waves through the arteries to measure how fast blood flows. The second method is the segmental Doppler pressure testing that checks various parts of the legs for blocked or narrowed arteries. The procedure is similar to the ABI test, but the ultrasound device will amplify the sound of blood flow, making it easy to measure blood pressure and diagnose peripheral arterial disease.
Angiography (venography)
Angiography is minimal invasive testing that helps to visualize and diagnose blockages inside veins and arteries. In this procedure, the physician will insert a thin tube that injects a special dye that enables blood vessels to appear on an X-ray. As the dye is introduced to the arteries and veins, fluoroscopy imaging captures the detailed images to see the extent of blockages in the arteries.
Blood Tests
Doctors also take a sample of your blood to measure the levels of cholesterol and triglycerides. Blood samples are also used to check for diabetes.
Magnetic Resonance Angiography (MRA)
MRA tests are conducted to examine the structure of the arteries in your leg. However, the doctor will speak to you before using the procedure. Magnetic resonance angiography is not recommended for people with metal implants in their bodies.
For more information on Vein and Vascular conditions, please check out our Youtube Channel.