Unlocking the Secrets of Peripheral Artery Disease (PAD)
LJVascular2024-10-07T06:02:49-07:00Unlocking the Secrets of Peripheral Artery Disease (PAD): A Comprehensive Guide
Peripheral Artery Disease (PAD) Unveiled: Understanding the Hidden Threat
Peripheral Artery Disease (PAD) is a critical yet often overlooked condition that affects millions of people worldwide, particularly those over the age of 50. This vascular disorder can lead to serious health complications if left untreated, making early diagnosis and intervention crucial. Understanding the risk factors, symptoms, and management options for PAD can empower individuals to take charge of their vascular health and prevent severe consequences.
In this comprehensive guide, we will explore what PAD is, how it develops, its key symptoms, risk factors, and why timely diagnosis and treatment are essential. We will also delve into modern approaches to managing PAD to help you make informed decisions for your health.
What is Peripheral Artery Disease (PAD)?
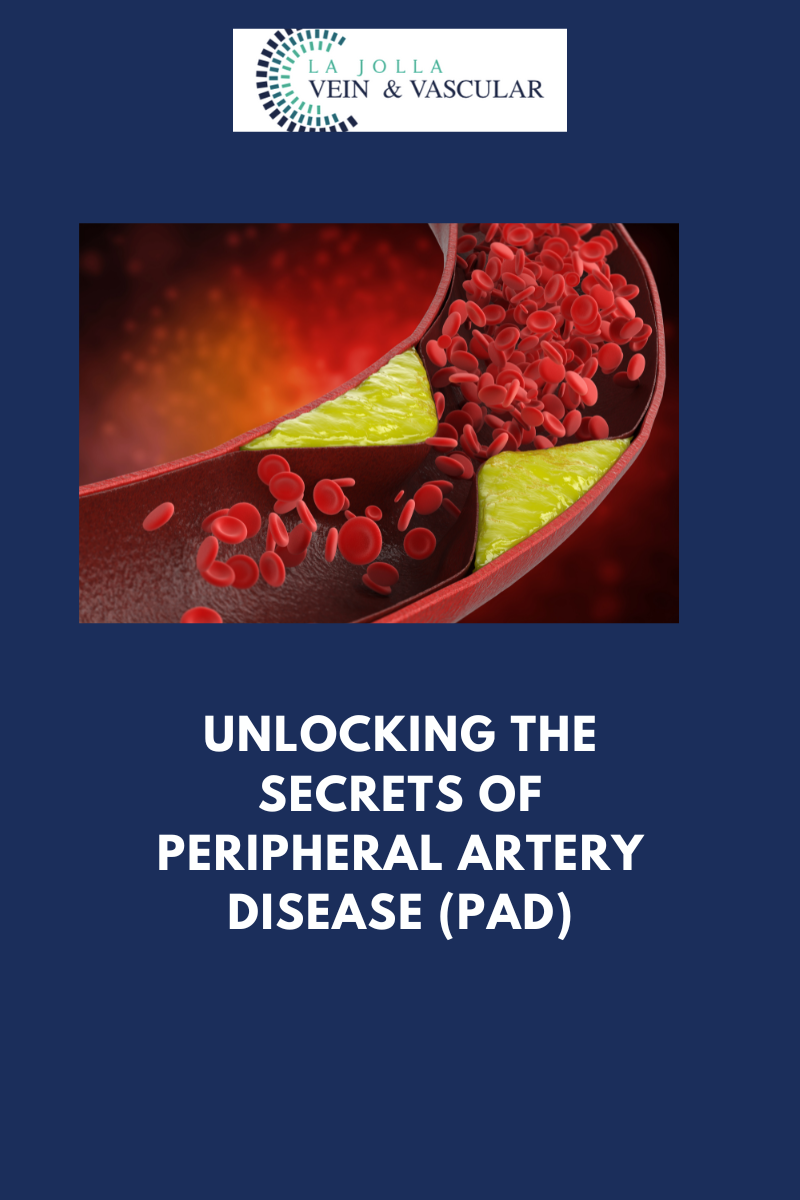
Peripheral Artery Disease (PAD) refers to the narrowing of arteries outside the heart, primarily in the legs and lower extremities. This narrowing is caused by the buildup of plaque, a substance made up of cholesterol, calcium, and other materials found in the blood. Over time, this accumulation restricts blood flow, depriving the tissues of oxygen and essential nutrients. The resulting condition not only causes discomfort but also increases the risk of severe cardiovascular events like heart attacks and strokes.
PAD often remains undiagnosed in its early stages because its symptoms can be subtle or attributed to aging or other conditions. However, recognizing the early signs is vital for preventing more serious complications down the line.
Peripheral Artery Disease Symptoms: Spotting the Early Warning Signs
The symptoms of PAD can vary depending on the severity of the condition and the arteries affected. One of the hallmark signs is intermittent claudication, which refers to muscle pain or cramping in the legs or hips during physical activity like walking or climbing stairs. This pain typically subsides with rest but returns when the activity is resumed.
Other common symptoms of PAD include:
- Leg numbness or weakness: This occurs due to reduced blood flow, leading to insufficient oxygen supply to the muscles.
- Coldness in the lower leg or foot: One leg may feel significantly colder than the other, indicating poor circulation.
- Sores on the toes, feet, or legs that won’t heal: Persistent wounds are a red flag for poor blood flow.
- Hair loss on the legs: A lack of nutrients can cause hair to thin or fall out in areas affected by PAD.
- Shiny skin on the legs: The skin may appear tight and shiny due to the lack of proper circulation.
- Weak pulse in the legs: A diminished pulse in the legs or feet can signal arterial blockages.
In more advanced cases, PAD can lead to critical limb ischemia (CLI), where the lack of blood flow causes severe pain, infections, and even gangrene, potentially leading to amputation.
What Causes Peripheral Artery Disease?
The primary cause of PAD is atherosclerosis, the same condition that causes coronary artery disease. In atherosclerosis, fatty deposits (plaque) accumulate on the inner walls of the arteries, restricting blood flow. Over time, these deposits harden and narrow the arteries, making it difficult for blood to pass through.
Several factors contribute to the development of PAD, including:
- Smoking: Tobacco use is one of the most significant risk factors for PAD. The chemicals in cigarettes can damage the lining of the arteries, leading to plaque buildup.
- Diabetes: High blood sugar levels can damage the blood vessels and increase the risk of plaque formation.
- High cholesterol: Elevated levels of bad cholesterol (LDL) contribute to plaque accumulation.
- High blood pressure: Hypertension weakens the arterial walls, making them more susceptible to atherosclerosis.
- Age: The risk of PAD increases with age, particularly after the age of 50.
- Sedentary lifestyle: Lack of physical activity can contribute to poor circulation and increase the likelihood of plaque buildup.
Diagnosing Peripheral Artery Disease: Why Early Detection Matters
Accurate and early diagnosis of PAD is essential for effective treatment and prevention of complications. A thorough medical evaluation, combined with diagnostic tests, can determine the severity of the disease and guide the appropriate course of action.
At La Jolla Vein & Vascular, our team of vascular specialists uses a variety of diagnostic tools to evaluate patients for PAD. These may include:
- Ankle-Brachial Index (ABI): This test compares the blood pressure in your ankle to the blood pressure in your arm. A lower pressure in the ankle indicates reduced blood flow, suggesting PAD.
- Doppler Ultrasound: This non-invasive test uses sound waves to measure blood flow in the arteries and identify any blockages.
- Angiography: This imaging test involves injecting a contrast dye into the arteries to visualize blood flow and locate narrowing or blockages.
- Magnetic Resonance Angiography (MRA): A type of MRI that provides detailed images of the arteries without the need for contrast dye in some cases.
By diagnosing PAD early, healthcare providers can recommend lifestyle changes, medications, or interventions that prevent the progression of the disease and reduce the risk of serious complications.
Managing Peripheral Artery Disease: Taking Control of Your Health
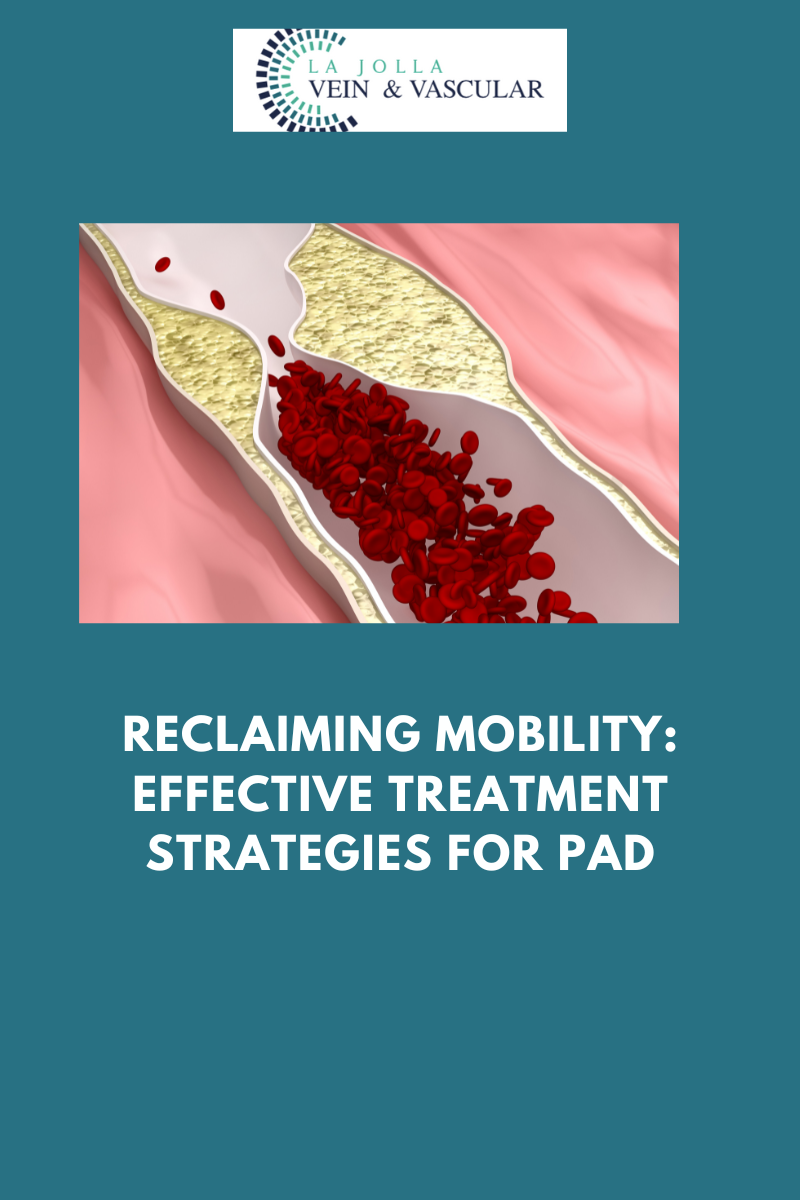
Once PAD is diagnosed, there are several strategies to manage the condition and improve circulation. Treatment depends on the severity of the disease and the patient’s overall health, but the primary goals are to relieve symptoms, prevent the progression of atherosclerosis, and reduce the risk of heart attack or stroke.
Lifestyle changes are often the first line of defense:
- Quit smoking: This is the single most effective way to slow the progression of PAD. Smoking cessation improves circulation and reduces the risk of complications.
- Exercise regularly: Walking, cycling, and other aerobic exercises can help improve blood flow and reduce symptoms of claudication.
- Eat a heart-healthy diet: A diet low in saturated fats, trans fats, and cholesterol can help reduce plaque buildup in the arteries.
- Manage diabetes and high blood pressure: Keeping these conditions under control is crucial for slowing the progression of PAD.
In more advanced cases, medications may be prescribed to manage symptoms and prevent complications. These might include blood thinners to prevent clots, medications to lower cholesterol, or drugs to improve blood flow in the legs.
In some cases, surgical intervention may be necessary to restore proper blood flow. Procedures like angioplasty or bypass surgery can open up narrowed arteries and improve circulation in affected areas.
Recommended for you: