La Jolla Vein and Vascular Treatments for Varicoceles
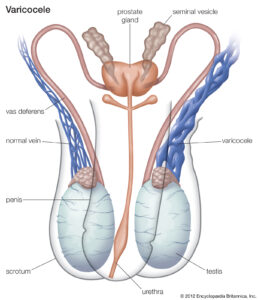
In most cases, varicoceles treatment is not necessary. Most men with varicoceles do not experience fertility issues. However, if the condition is causing pain, testicular atrophy, or infertility, you can benefit from varicoceles treatment. The treatment helps in sealing off the affected vein and redirecting the blood flow into normal veins. In case of infertility issues, varicoceles treatment helps in improving the quality of the sperm and sperm count. The procedure that we perform at LA Jolla Vein & Vascular on varicocele is percutaneous embolization of varicocele embolization.
The primary goal for varicocele treatment procedures is to help prevent the backflow of blood from the body to the scrotum, helping in cooling off the testes. Surgical procedures will help restrict the blood flow to the veins leading from the testis to the body. However, not all the veins are sealed off. The vassal vein, which is not subject to the same problems as the other varicose veins, is left open to allow blood to leave the testicles after the procedure.
Some of the clear indications that you need varicoceles repair during adolescence include pain, progressive testicular atrophy, and abnormal semen analysis results. While this treatment helps in improving sperm characteristics, it is not clear whether untreated varicoceles can lead to progressive sperm worsening. The common varicoceles treatment options include (La Jolla Vein & Vascular Only Performs Varicocele Embolization):
Percutaneous Embolization (Varicocele Embolization)
Percutaneous embolism is an advanced procedure performed by a radiologist. The specialist usually makes a small cut into a vein in the groin and inserts a tube. The doctor will use X-ray imaging to guide them to the affected veins and insert a coil or a balloon into it through the tube. The procedure helps in blocking the blood flow to the varicocele, shrinking it gradually. This procedure is also done with general anesthesia.
Catheter-directed Embolization
Catheter-directed embolization is a non-surgical, outpatient treatment performed by an interventional radiologist using imaging to guide catheters or other instruments inside the body. Through mild IV sedation and local anesthesia, patients are relaxed and pain-free during the approximately two-hour procedure.
For the procedure, an interventional radiologist makes a tiny nick in the skin at the groin using local anesthesia, through which a thin catheter (much like a piece of spaghetti) is passed into the femoral vein directly to the testicular vein. The physician then injects contrast dye to provide direct visualization of the veins so he/she can map out exactly where the problem is and where to embolize or block the vein, which reduces pressure on the varicocele. By embolizing the vein, blood flow is redirected to other healthy pathways. Essentially, the incompetent vein is shut off internally by preventing blood flow, accomplishing what the urologist does without surgery.
Efficacy of Embolization for Varicoceles
Embolization is equally effective in improving male infertility and costs about the same as surgical ligation. Pregnancy rates and recurrence rates are comparable to those following surgical varicocelectomy. In one study, sixty percent conceived were treated for infertility.
In another study, sperm concentration improved in 83 percent of patients undergoing embolization compared to 63 percent of those surgically ligated. Patients who underwent both procedures expressed a strong preference for embolization.
Varicocelectomy
Your doctor will make a small 1-inch incision into your scrotum and use a microscope or magnifying glass to see the veins better. The doctor might use local anesthesia to numb the area. General anesthesia can also help you sleep through the procedure.
Laparoscopic Surgery
This procedure involves making a much smaller incision and inserting a tube that holds the surgical tools. The surgeon will also use a special camera to see inside you. The procedure is done under general anesthesia to help you sleep through the procedure. The results from the other treatments are similar, only that the incision is small with laparoscopic surgery.
Open Surgery
The open surgery treatment is usually done on an outpatient basis and using a local or general anesthetic. The surgeon will make a small incision below your groin or abdomen to access the affected vein. Your doctor uses advanced surgical tools such as Doppler ultrasound and a surgical microscope to help guide the procedure. The patient can return to a regular daily routine after two days.
Recovery
In most cases, you can go back to your routine after two days of varicose treatment. However, it is advisable to take it easy. Avoid strenuous activities and exercise for about two weeks.
People who have undergone percutaneous embolization tend to recover faster. While you may need a day or two off from work, you can return to your workout program in 7-10 days. If the treatment procedure is to help with fertility, your doctor will perform an additional test in 3-4 months. You will be able to see improved results in 6-12 months. It is important to note that more than 50 percent of men who have undergone the procedure have restored their fertility. Additionally, these surgical procedures are also crucial for teens as they help in slowing testicular growth.
For more information on vein and vascular treatment please visit our YouTube Channel.