Complications of Untreated Varicose Veins: Bleeding or Hemorrhage Caused by Vein Rupture
LJVascular2022-09-19T15:41:12-07:00Untreated varicose veins are at a higher than usual risk of bleeding or spontaneous rupture. Over time, varicose veins become larger, and the vein wall becomes weak and stretched out. These veins, which are already weak, are also under high pressure (because of venous reflux, or the ‘backflow’ and pooling of blood in these veins). As a result, the high pressure can cause the veins to spontaneously burst and bleed heavily. Because they are under high pressure, they bleed like an arterial bleed and patients describe the bleeding as ‘blood shooting across the room.’
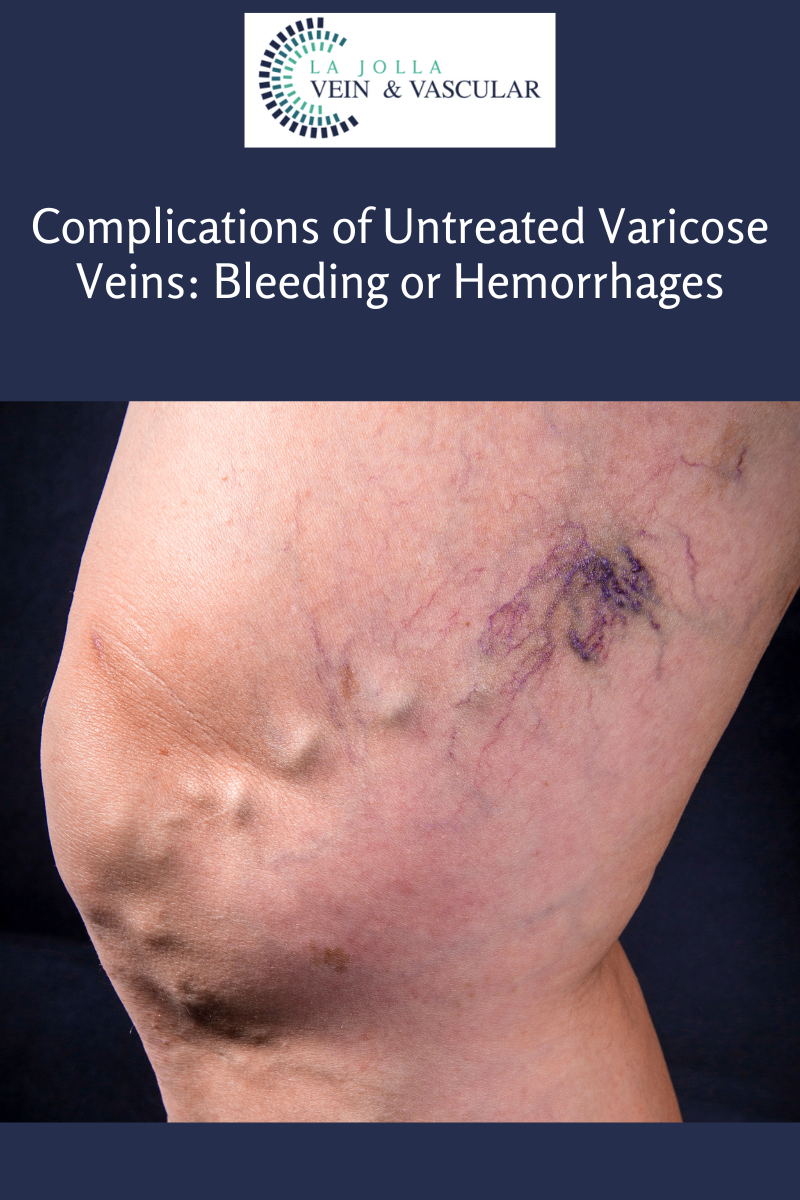
The varicose veins that are susceptible are veins closest to the surface of the skin.
Most patients describe that it occurs during or after a warm shower (warm water causes veins to relax and dilate, allowing more blood to pool within the veins) or during sleep. It is painless and patients report that they notice it because they feel something wet in bed. Patients who are on blood thinners can lose large amounts of blood, especially if it occurs while they are sleeping. Some people have required blood transfusions. The small blue spider veins around the ankle are equally at risk of rupture as are the larger bulging veins.
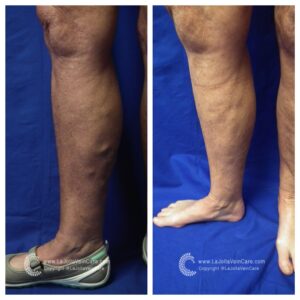
This is a patient who experienced spontaneous hemorrhage of their varicose veins. Notice the appearance of the blue, bulging veins that we describe as, ‘blue blebs.’ These veins are dilated, weak, and are close to the surface of the skin. The pooling blood within these veins causes high pressure, ultimately resulting in a spontaneous rupture or hemorrhage. The bleeding is rapid since varicose veins are under high pressure. This is a common condition that we see at La Jolla Vein Care.
If someone you know has experienced bleeding from their varicose veins, they should be seen by a doctor. Treatment will prevent the veins from bursting again. This is a common condition that we see at La Jolla Vein & Vascular.
“Bringing Experts Together for Unparalleled Vein and Vascular Care”
La Jolla Vein & Vascular (formerly La Jolla Vein Care) is committed to bringing experts together for unparalleled vein and vascular care.
Nisha Bunke, MD, Sarah Lucas, MD, and Elliot DeYoung, MD are specialists who combine their experience and expertise to offer world-class vascular care.
Our accredited center is also a nationally known teaching site and center of excellence.
For more information on treatments and to book a consultation, please give our office a call at 858-550-0330.
For a deeper dive into vein and vascular care, please check out our Youtube Channel at this link.
For more information on varicose veins and eliminating underlying venous insufficiency, check this link out full of resources.