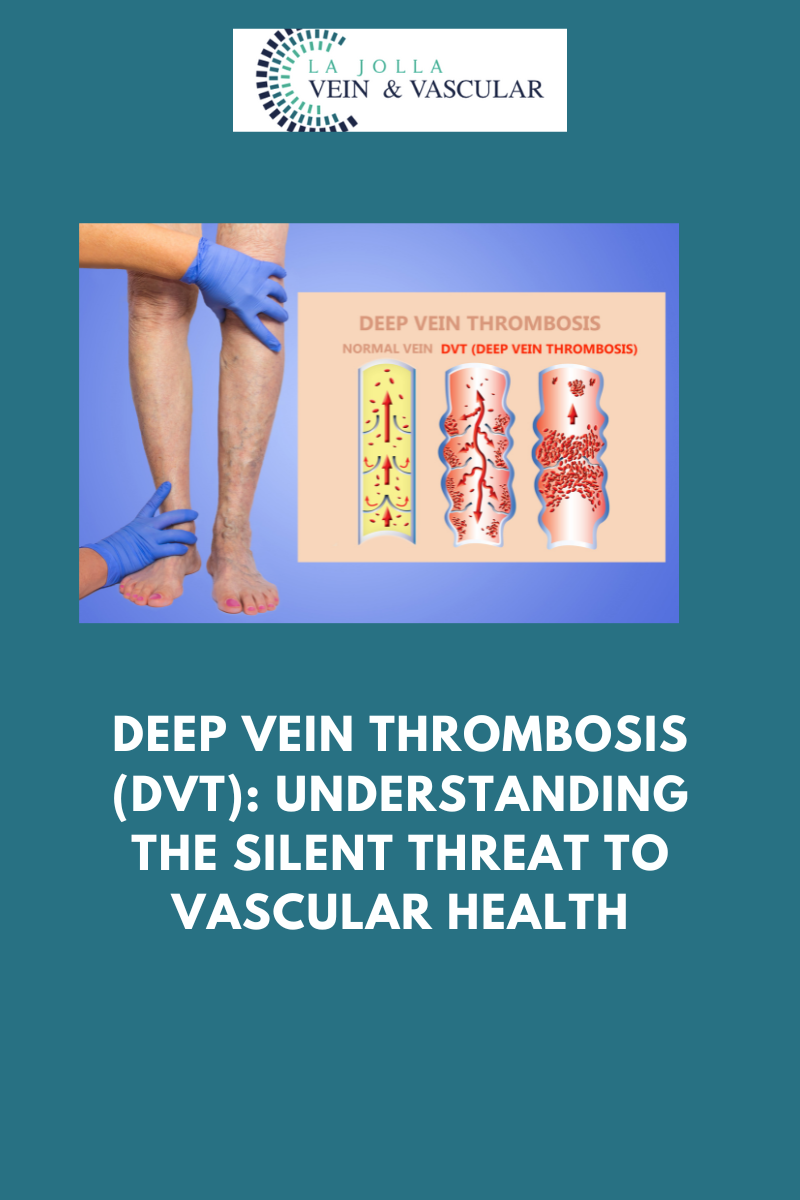
Deep Vein Thrombosis (DVT): Understanding the Silent Threat to Vascular Health
LJVascular2024-07-06T22:49:37-07:00Deep Vein Thrombosis (DVT): Understanding the Silent Threat to Vascular Health
Deep Vein Thrombosis, more commonly known as DVT, is a medical condition characterized by the formation of blood clots deep within the veins of the lower extremities. While these clots may remain concealed beneath the surface, the lurking danger […]