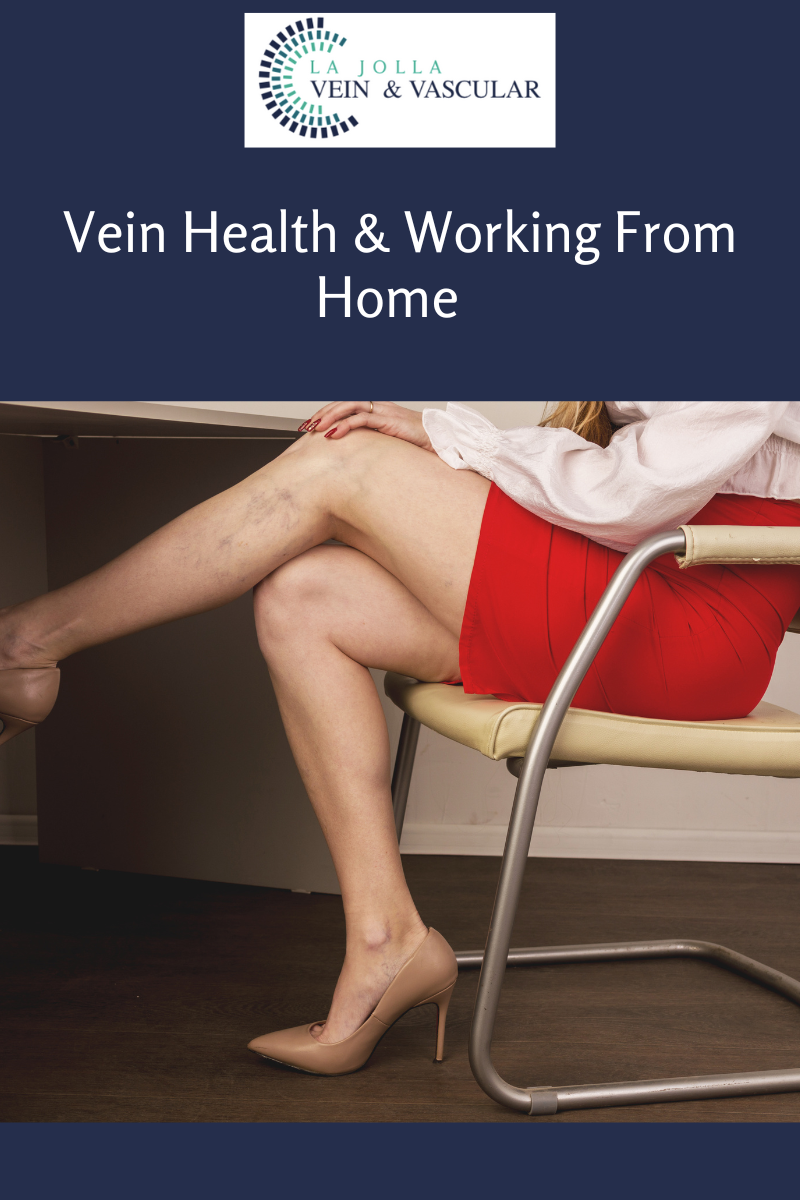
Vein Health & Working From Home
LJVascular2022-12-13T13:18:14-08:00Prolonged desk work can increase the risk of blood clots in leg veins and decline your vein health.
As many Americans are working from home, we have received many calls from patients regarding thrombophlebitis, which is a big concern for vein health. This is not a new scenario for us, over the […]