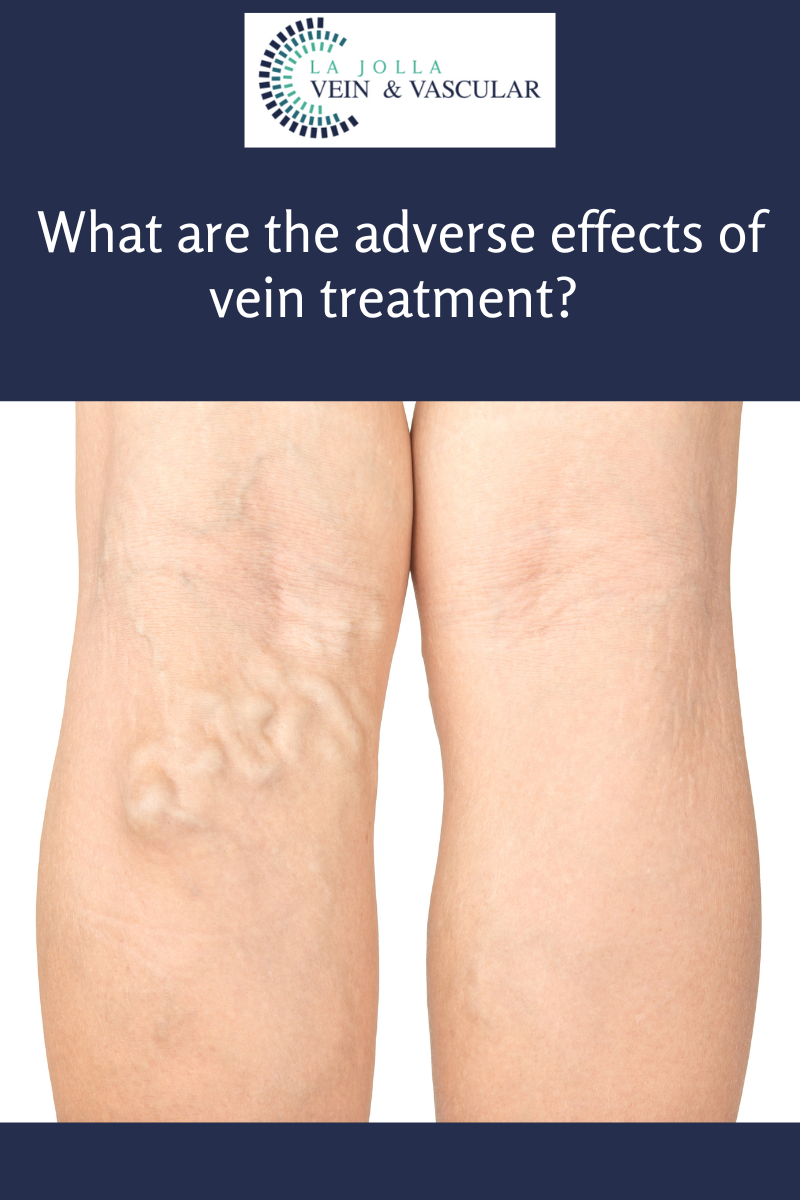
What are the adverse effects of vein treatment?
LJVascular2022-06-25T15:48:17-07:00Adverse effects of vein treatment are uncommon, but they can occur. Below are some signs to look out for if you have recently had vein treatment.
Patients generally do very well with vein treatments, all of which have a low risk of complications. Most patients feel the benefits within a couple of […]