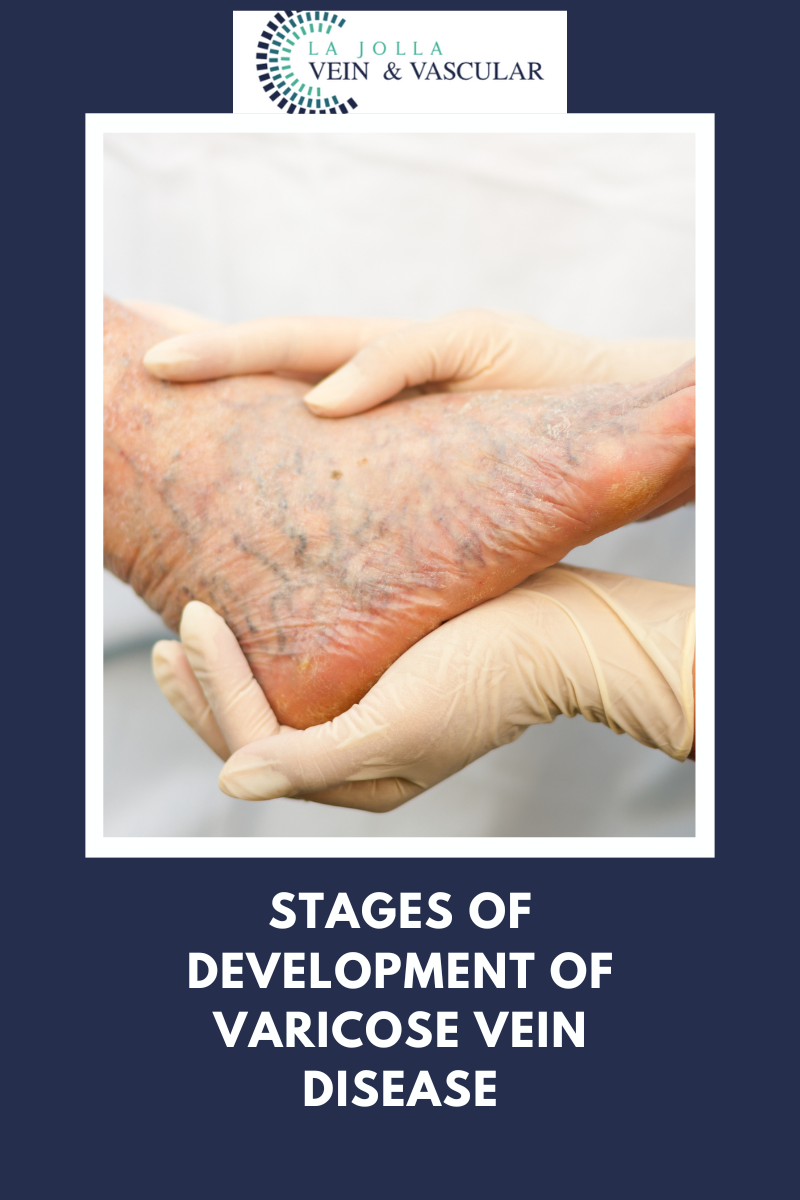
Stages of development of varicose veins
LJVascular2023-02-13T15:23:17-08:00Venous reflux disease is also known as venous stasis, venous insufficiency or venous incompetence. Venous reflux disease refers to ‘leaky valves’ in the veins of the legs. Reflux may occur in the deep and/or superficial leg veins. The deep veins are those within the muscle; they bring at least 80-90% of the blood […]