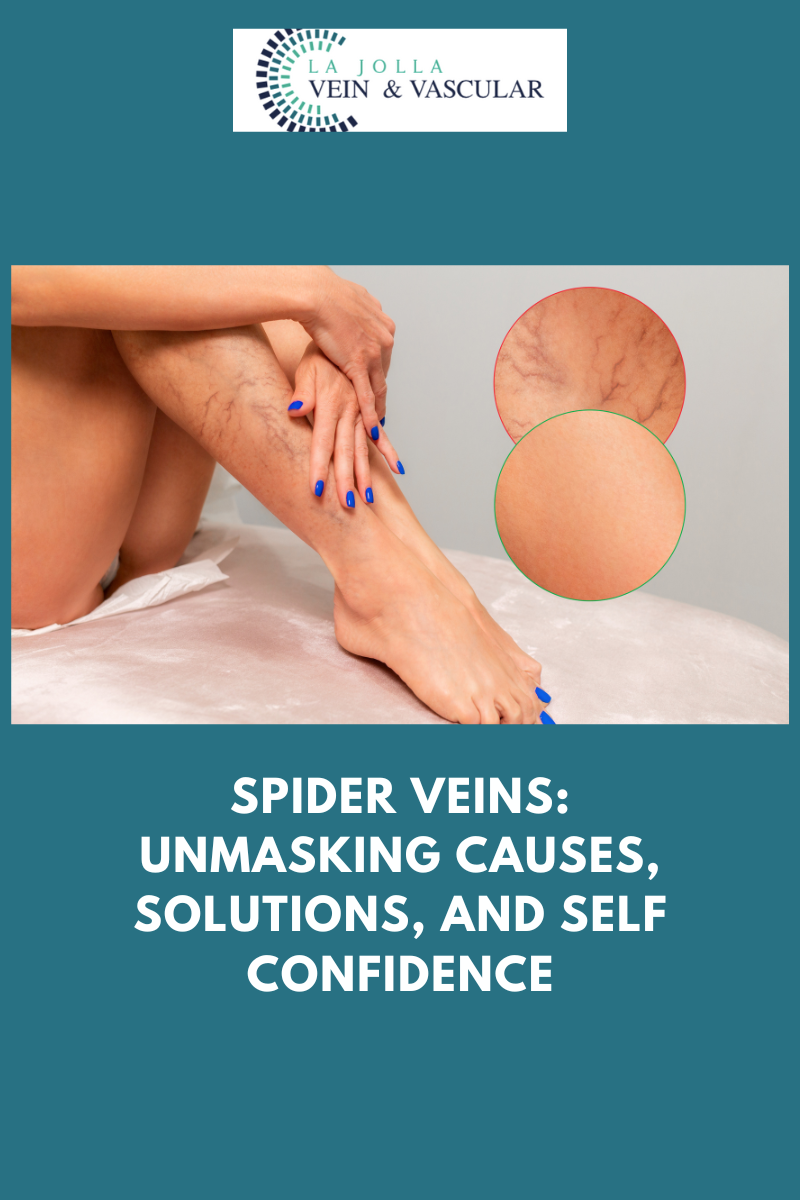
Spider veins: unmasking causes, solutions, and self confidence
LJVascular2024-07-06T18:28:22-07:00Spider veins: unmasking causes, solutions, and self confidence

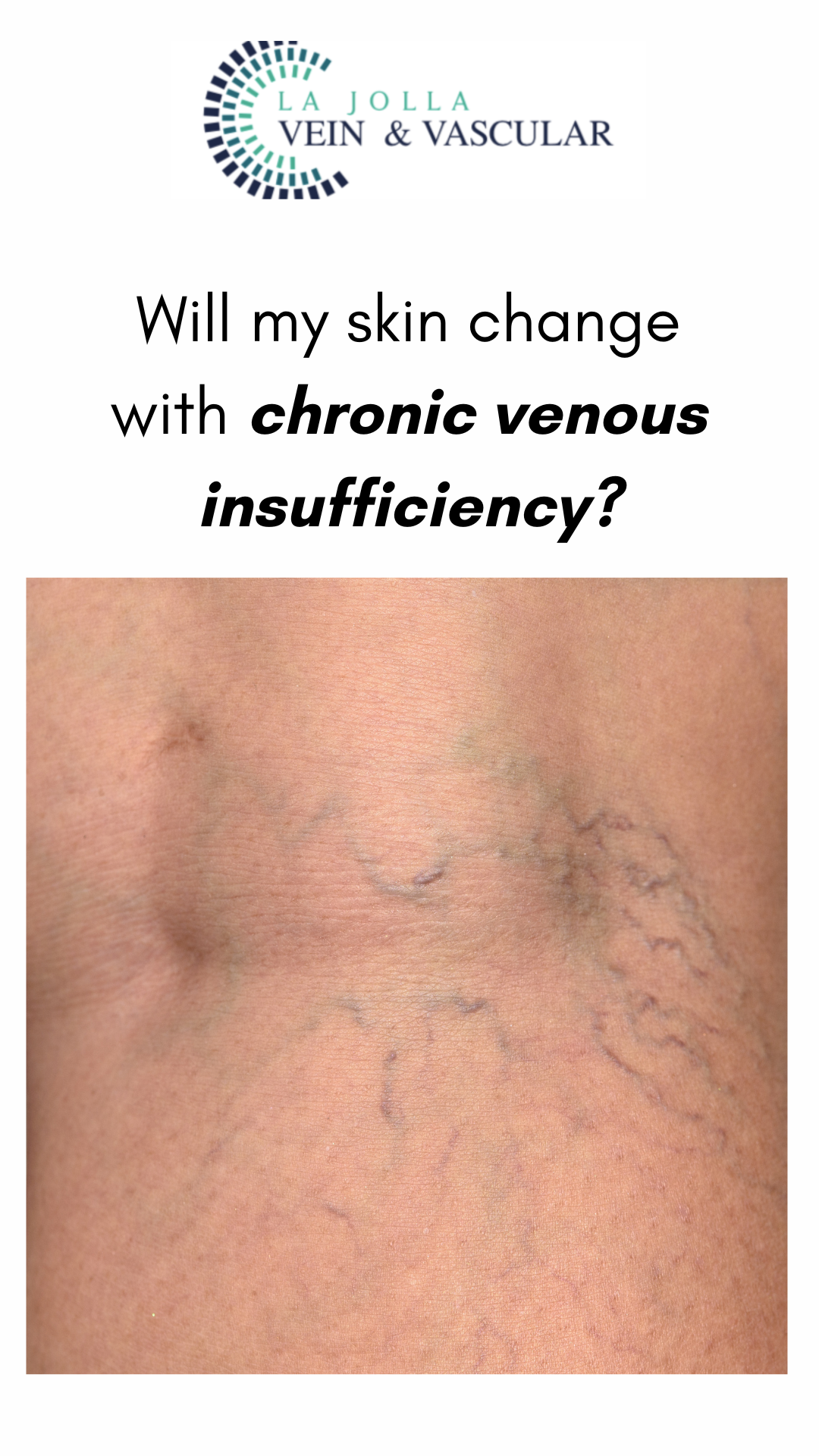
Spider veins, those delicate veins with their intricate web-like patterns on the skin’s surface, are often viewed as primarily a cosmetic concern by many. However, beneath their […]





![What do I need to know about venous disease? 11 What Do I Need to Know About Venous Disease? [2024]](https://ljvascular.com/wp-content/uploads/2024/03/Bunke-March-Blog-Thumbnail-37.png)