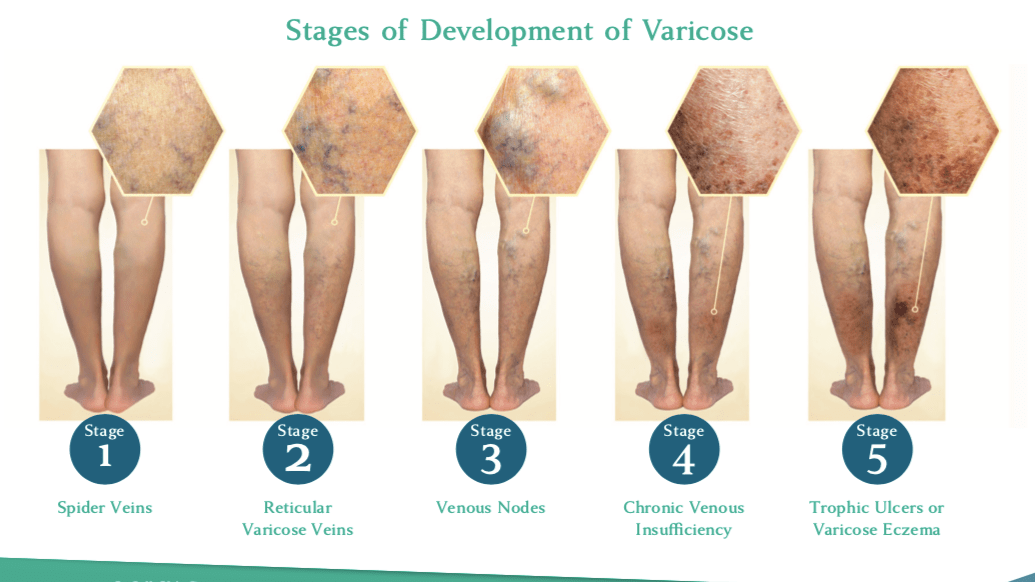
Spider Veins Along the Ankle Indicate Underlying Reflux Disease
Nisha Bunke2025-09-04T12:45:03-07:00Bluish and red-colored spider veins along the inner ankle and foot are referred to as corona phlebectasia in the vein world. This description refers to the ‘crown’ or cluster like distribution of these small blood vessels. Spider veins are often falsely considered as a cosmetic issue. But on the contrary, the presence of corona […]