What is Uterine Fibroid Embolization (UFE)
With modern medication and care, conditions like fibroid tumors have become more treatable and easier to manage. Uterine Fibroid Embolization (UFE), for instance, is a fairly straightforward procedure used in the treatment of fibroid tumors in the uterus.
Sometimes referred to as uterine artery embolization (UAE), the uterine fibroid embolization (UFE) procedure helps countless women plagued by fibroid tumors.
What does the uterine fibroid embolization treatment entail, and how can you prepare for the procedure? Here’s everything you need to know about uterine fibroids treatment.
What is Uterine Fibroid Embolization?
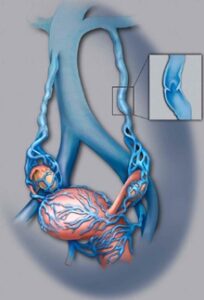
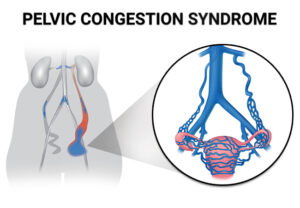
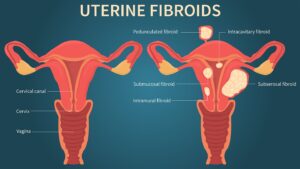
The muscular walls of the uterus can sometimes be invaded by non-cancerous fibroid tumors. These tumors are also known as myomas and are a form of benign tumors. While these fibroid tumors rarely become cancerous, they can lead to other severe conditions such as increased menstrual bleeding, bowel or bladder pressure, and pelvic discomfort.
Admittedly, while uterine fibroid embolization shows a high success rate, more research is still needed on the subject. For instance, at the moment, the procedure is usually performed on women who no longer desire to get pregnant. The UFE procedure may also be used on women who wish to avoid a hysterectomy procedure.
When is Uterine Fibroid Embolization Used?
As mentioned above, uterine fibroid treatment is rather straightforward and minimally invasive. As a result, the procedure can be used in a wide variety of cases. Some of the instances where the treatment is necessary or advocated for include;
- Malignant gynecological tumors
- Hemorrhage after childbirth
- General or specific trauma
How to Prepare for a Uterine Fibroid Embolization Procedure
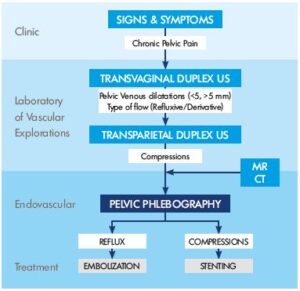
The healthcare professional will first need to ascertain if the fibroid tumors are the underlying cause of any visible and diagnosable symptoms. Afterward, they’ll need to determine the size, location, and the number of fibroids. This can be done with the help of an ultrasound machine or magnetic resonance imaging (MRI) equipment.
Moreover, your gynecologist may also need to run a physical examination through a laparoscopy examination. This test gives a clearer picture of the uterus and the invasive fibroids. You could also have a biopsy of the inner lining of the uterus if you are bleeding excessively in between your periods. The procedure known as endometrium helps rule out cancer as the cause of bleeding.
If you are on any medication, supplements, or herbal remedies, you’ll need to inform the doctor before the procedure. Additionally, make a list of any known allergies, including general and local anesthesia and the dye or contrast materials.
It’s also wise to notify the healthcare team if you have recently suffered an illness, just finished treatment, or are on other medication. For example, if you’re on blood thinners, the healthcare provider may advise you temporarily halt the medication in preparation for the procedure.
Women who suspect they are pregnant should let the doctor know well before the uterine fibroid embolization treatment. Some imaging tests are usually not performed during pregnancy in a bid to minimize any radiation exposure to the fetus. In the case of an imaging test, such as an x-ray, which is essential to the operation, particular care guidelines must be followed to manage and reduce radiation exposure.
While preparing for the procedure, you’ll likely be put off solid meals after midnight to the procedure’s day. While the procedure takes a few hours, the doctor could request to stay overnight for further observation.
What Equipment to Expect
Since this is a minimally invasive procedure, the tools and equipment used are reasonably common and risk-free. Some of the equipment to be used in uterine fibroid embolization treatment includes a catheter, x-ray machines, and various embolic agents and medications.
The synthetic material used is known as embolic agents and varies in composition and efficacy. The three most common types of embolic agents are;
-Gelfoam whose texture resembles spongy material
-Polyvinyl alcohol, which resembles coarse sand
-Microspheres, which is a polyacrylamide sphere coated with gelatin
These tolls, equipment, and medication are all safe to use during the uterine fibroid embolization treatment.
Benefits and Risks Associated with Uterine Embolization Treatment
Some of the advantages of uterine fibroid embolization include;
-There’s no need for surgery as the procedure is minimally invasive
-You can resume regular activity sooner and faster
-The procedure is highly effective, boasting well over 90% efficacy rating
-Fibroids rarely regrow after the uterine embolization treatment
-On the other hand, some of the risks that could occur during the procedure are;
-The procedure pierces the skin and could leave an infection if not properly cleaned
-The embolic agents need to be guided carefully, or they could lodge in the wrong area
-Fibroids can lead to chronic pain and an array of other conditions. With uterine embolization treatment, you can now get relief and get back to your healthy self.
What To Expect during Uterine Fibroid Embolization Procedure
A UFE usually takes between 1 and 3 hours and patients usually require about 6 hours of bed rest after the procedure. Patients may experience mild discomfort as the embolization takes full effect. The fibroid tumors breaking down and exiting the body may cause light bleeding for the few weeks after the procedure. Most patients can expect to return to normal activity 7 to 10 days after the procedure. Our physicians will most likely recommend a follow-up consultation after the UFE 1 to 3 weeks afterward and an ultrasound or MRI 3 to 6 months later to monitor your progress.