Our new La Jolla Vein & Vascular Vista Clinic is now open!!!
LJVascular2023-05-30T17:32:05-07:00Our new La Jolla Vein & Vascular Vista Clinic is now open!!!

We had our wonderful ribbon cutting ceremony this past month with Vista City’s Chamber of Commerce.

We were so honored to have Vista City Council member, Dan O’Donnell and
District Representative, Jessica Ramirez attend and support our opening!


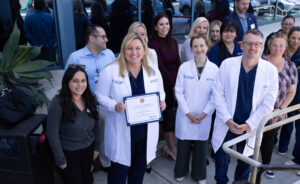
Thank you to all who attended. We are proud and honored to serve the Vista community! Stay tuned for more updates from the clinic through our social media and website and special informational posts to learn more about what we specialize in and can help you with!
North County San Diego / Vista Endovascular Center
Location: Our North County office is located on the south side of Highway 78 in Vista, East of I-5 and 6 miles from Tri-City Medical Center. It is just miles from Oceanside and Carlsbad. Our endovascular center is located at this location.
-Phone: 760-249-7007
-Text us: (858) 283-4099
-Fax: (760) 249-7017
-Full Address: 906 Sycamore Ave, Vista, CA 92081
Vista Clinic Services:
-Vascular lab & Diagnostic Imaging:
La Jolla Vein and Vascular’s non-invasive vascular laboratory utilizes advanced imaging machines that look for vascular diseases that may affect how well blood flows in the arteries and veins. As an accredited Vein Center, we are expanding our services in vascular imaging to offer comprehensive diagnostic vascular testing. Our laboratory is accredited by the Intersocietal Accreditation Commission (IAC) for Vascular Testing.
-Evaluation for all vascular conditions of the legs, feet and pelvis
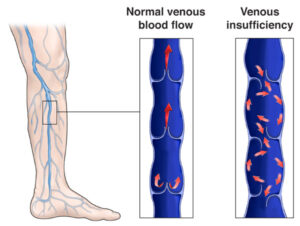
The vascular lab examines blood vessels throughout the body that feed major organs and tissue. These tests can help diagnose and treat many vascular conditions such as peripheral arterial disease (PAD), stroke, aneurysms and venous insufficiency.
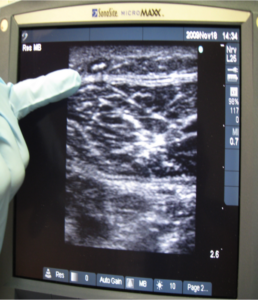
By using cutting edge diagnostics, our Duplex Ultrasound technology is used for screening and testing purposes.
A Duplex ultrasound combines Doppler flow information and conventional imaging information, sometimes called B-mode, to allow physicians to see the structure of your blood vessels. Duplex ultrasound uses sound waves to get images of your blood vessels. It also helps determine how fast blood moves through the vessels. It can also be useful to estimate the diameter of a blood vessel as well as the amount of obstruction, if any, in the blood vessel. Using duplex ultrasound technology, the structure of your blood vessels, the valve function, the movement of your red blood cells and direction of blood flow through the vessels, and any blockages or blood clots can be seen.
-Varicose vein procedures
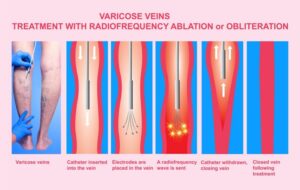
Step 1: The Underlying Problem
The first step is to treat the underlying problem, the venous reflux. The specific pattern of venous reflux was detected by ultrasound. Venous reflux usually starts in the saphenous veins. The saphenous veins are most effectively treated with vein ablation procedures. This involves placing a small catheter within the vein and using heat or a solution to produce injury and eventual closure of the vein. The most commonly used treatments for the saphenous veins are radiofrequency ablation (RFA), laser ablation, mechanico-chemical ablation
(MOCA or Clarivein), and in some cases Varithena Foam or Venaseal.
The treatment recommendation is customized, based on where reflux is present and other factors that need to be considered when making this decision.
These will involve the following:
Your age, overall health, and medical condition.
Extent of the condition.
The findings of your venous ultrasound.
Your signs and symptoms.
Your tolerance of specific medicines, procedures, or therapies.
Expectations for the course of the condition.
Your opinion or preference.
Step 2: Varicose Vein Treatment
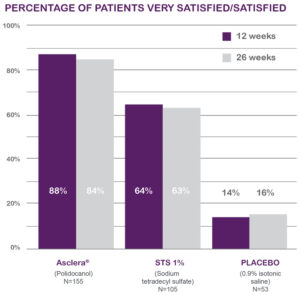
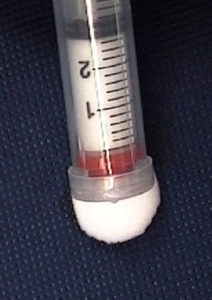
After the underlying saphenous vein reflux is corrected, the bulging veins (varicose veins) can be treated by injecting a foamed medication that will cause them to scar and eventually dissolve (foam sclerotherapy), or to remove them using tiny incisions. The most common method is foam sclerotherapy. This is also known as ultrasound-guided foam sclerotherapy (UGFS). Phlebectomy is another option which includes making small incisions to remove the vein.
-Leg ulcers
We might all be familiar with ulcers in a general manner, but certain types of ulcers behave quite differently due to various contributing factors. These are nonhealing ulcers or nonhealing wounds, and if not treated with care and in good time, such wounds can pose a serious risk to the patient’s health. Severe cases may lead to amputation of the affected limbs or loss of life in the most extreme circumstances. The nonhealing ulcers cases we treat here at La Jolla Vein & Vascular fall under peripheral arterial disease (PAD) and a subcategory of arterial disease.
Non-healing wounds or ulcers do not follow the usual healing process and are referred to as chronic wounds should they persist beyond 3 weeks. Such wounds can be a heavy burden to live with for anyone. Still, the board-certified vascular surgeons and specialists at La Jolla Vein & Vascular are dedicated to administering effective treatment and management solutions to all patients so they may resume a healthy, productive, and pain-free life.
-Lymphedema care
At La Jolla Vein & Vascular, we can assist in the diagnosis of a vascular cause of leg swelling by using duplex ultrasound. Duplex ultrasound can diagnose a blood clot or venous reflux. In some cases a venogram may be recommended if an obstruction higher than the groin is suspected. Lymphedema is a clinical diagnosis, but lymphoscintigraphy can be ordered at an outside imaging center.
-Endovascular Center (vein and arterial procedures)
Vista Clinic Providers:
-Dr. Elliot DeYoung (Interventional Radiologist)

Dr. Elliot DeYoung is a board-certified interventional radiologist who has spent his career focused on minimally invasive procedures. He completed his training at University of California, San Diego where he specialized in vascular interventions and served on the patient safety committee. Dr. DeYoung’s expertise spans vascular disease from angioplasty and stenting to embolization and ablation. He values thorough patient education and the continuity of patient care.
He will lead the center in the expansion of vascular services to provide crucial out-patient care to the community. The practice is enthusiastic to offer treatments for peripheral arterial disease, May Thurners’, and uterine fibroids.
Dr. DeYoung received his bachelor’s degree from USC in Psychology followed by his medical degree from the University of Sydney, School of Medicine. He initially trained as a General Surgery resident in New York before transitioning his training to Interventional Radiology in San Diego. He has a passion for water sports and his free time is spent enjoying the outdoors with his family.
Dr. DeYoung is looking forward to treating your vascular needs at La Jolla Vein & Vascular.
Our La Jolla Vein & Vascular Vista team is looking forward as well to serving you!

“Bringing Experts Together for Unparalleled Vein and Vascular Care”
La Jolla Vein & Vascular (formerly La Jolla Vein Care) is committed to bringing experts together for unparalleled vein and vascular care.
Nisha Bunke, MD, Sarah Lucas, MD, and Elliot DeYoung, MD are specialists who combine their experience and expertise to offer world-class vascular care.
Our accredited center is also a nationally known teaching site and center of excellence.
For more information on treatments and to book a consultation, please give our office a call at 858-550-0330.
For a deeper dive into vein and vascular care, please check out our Youtube Channel at this link, and our website https://ljvascular.com
For more information on varicose veins and eliminating underlying venous insufficiency,
Please follow our social media Instagram Profile and Tik Tok Profile for more fun videos and educational information.
For more blogs and educational content, please check out our clinic’s blog posts!