Telemedicine and Mobile Ultrasound Services Made Available throughout Southern California in an Aim to Ensure Important Health Concerns Don’t Go Untreated While Many Continue to Shelter in Place
LA JOLLA, CALIF. (June 9, 2020) – La Jolla Vein Care (LJVC), a leader in vein treatment serving the Southern California community for more than a decade, is actively working to enhance its traditional service offerings to assist new and existing clients amid the unprecedented times brought forth by COVID-19. In a world of social distancing and self-quarantine, many individuals are postponing medical care in a bid to reduce virus exposure levels – a move many healthcare experts anticipate may lead to worsening symptoms and potentially dangerous complications down the line. To offset the concern that underlying vein diseases will go unchecked to the detriment of patient well-being while also addressing the public desire to avoid unnecessary outings; La Jolla Vein Care has deepened its commitment to best-in-class telemedicine offerings and has recently launched a new mobile ultrasound service.
“House calls are something many people see as a thing of the past, but with the inactivity of self-quarantine potentially exacerbating underlying vein diseases combined with an overall reluctance to venture out to visit a doctor, we knew something needed to be done,” said Dr. Nisha Bunke, MD, FACPh, RPhS, venous disease specialist and vein clinic medical director at La Jolla Vein Care. “We’re proud to roll out these new service offerings to meet patient needs and adapt to changing preferences during this difficult time.”
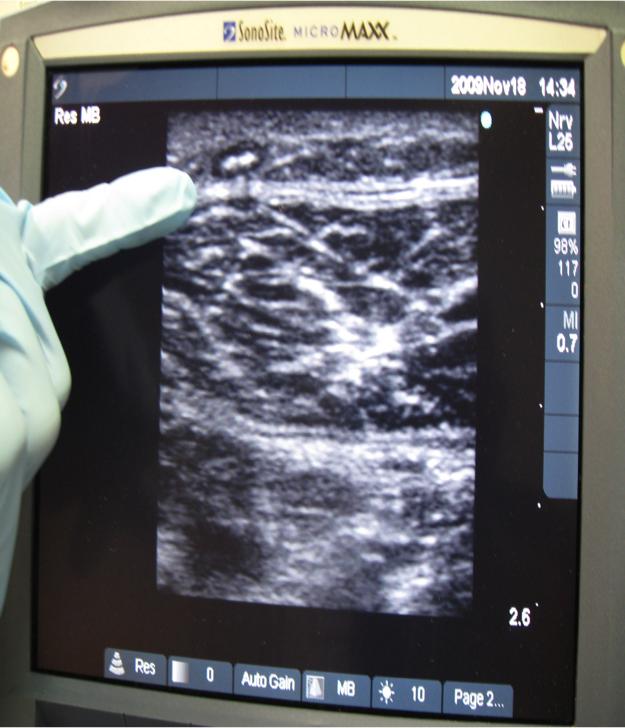
While varicose veins may be unsightly, they are not simply surface-level ailments and an ultrasound exam is required to diagnose the underlying venous diseases that cause these issues.
When left unchecked, the conditions can lead to chronic ailments like venous ulcers, but many people suffer from acute complications such as thrombophlebitis (blood clots within the veins), spontaneous vein hemorrhage, and disabling leg pain– so appropriate treatment should not be delayed, if at all avoidable.
As the first company of its kind to offer direct care to patients in their homes, La Jolla Vein Care has adopted the use of both telemedicine and state-of-the-art mobile ultrasound services via Terason uSmart 3300 NextGen technology. While telemedicine was quickly made available for consultations, pre-procedure assessments and post-procedure follow up appointments, the treatment center is advancing its accessibility initiative through new in-home mobile ultrasound diagnostics conducted by certified technicians – ushering in a new era of vein care.
Patient safety is at the forefront of LJVC’s new mobile service offerings – from the utilization of hospital-grade cloud storage systems, to cutting-edge technology that allows doctors to view results safely from a distance and adherence to all CDC guidelines including temperature checks and personal protective equipment (PPE).
Most assessments will begin with a telemedicine “visit,” followed by a mobile ultrasound screening in the patient’s home, spanning a wide radius of service area ranging from Chula Vista to San Juan Capistrano. If an in-office procedure is deemed necessary, temperature checks, ample PPE, and multiple hand-washing and sanitizing stations are available before coming into the building—and even then, only one patient will be allowed in the office at a time. Patients can conveniently wait in their cars until they are notified by text that their examination room is available.
Telemedicine and tele-radiology services are currently available to patients without additional convenience fees. LJVC accepts most PPO insurance types and considers itself now ready for the new normal of non-emergency medicine.
To book a telemedicine consultation with La Jolla Vein Care, visit https://ljvascular.com/or call (858) 550-0330.