Patient spider veins transformations
LJVascular2024-10-31T19:54:38-07:00Patient Spider Vein Transformations
Spider veins, those delicate reddish veins that grace the skin’s surface, can sometimes be more than just a cosmetic concern. In this blog post, we’ll explore what spider veins are, delve into their symptoms, uncover their underlying causes, and shed light on the importance of effective treatment.
What are Spider Veins?
Spider veins, often referred to as thread-like veins, are those fine, reddish veins that can be seen just beneath the skin’s surface. While they are commonly associated with cosmetic issues, they can hint at underlying problems that might require attention. These visible veins are not a sign of healthy circulation.
Unveiling the Underlying Issues
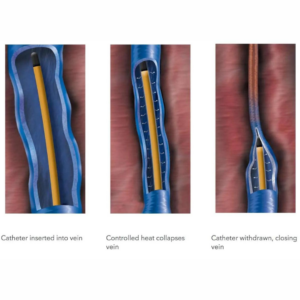
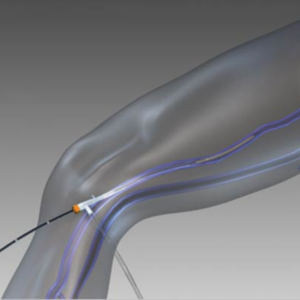
Beneath the surface, feeder veins, also known as ‘reticular veins‘ or ‘blue veins,’ can be the culprits behind the appearance of spider veins. These feeder veins, not visible to the naked eye, provide the pathways through which spider veins arise. It’s important to note that spider veins might also be indicative of venous insufficiency. For instance, if spider veins appear around the inner ankles or inner thighs, it could signal an underlying issue with the saphenous vein. In such cases, seeking an ultrasound examination is recommended to pinpoint and treat the root cause effectively.
Spotting the Symptoms
Spider veins can affect individuals in diverse ways. For some, they might be a painless aesthetic concern, while for others, they could lead to discomfort. The most commonly reported symptoms associated with spider veins include burning sensations, throbbing, localized pain, and feelings of heat and itchiness. In more severe cases, spider veins might even bleed.
Peering into the Causes
Spider veins on the legs share a common cause with varicose veins. Both conditions result from leaky vein valves that allow blood to pool within the veins, leading to their stretching and enlargement. On other parts of the body, such as the face and chest, factors like sun damage, hormonal fluctuations, or liver disease can trigger the appearance of spider veins. Hormonal changes, like those occurring during pregnancy, as well as the use of birth control or hormone replacement therapy, can weaken vein walls and contribute to their emergence.
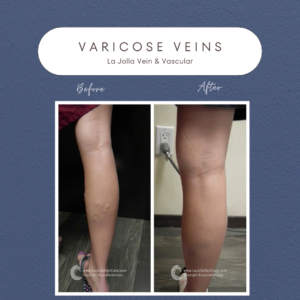
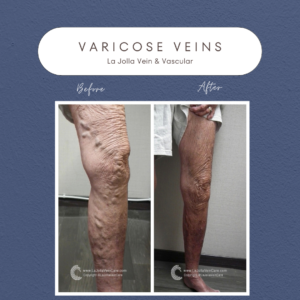
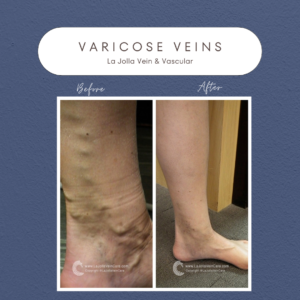
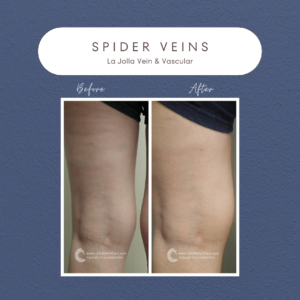
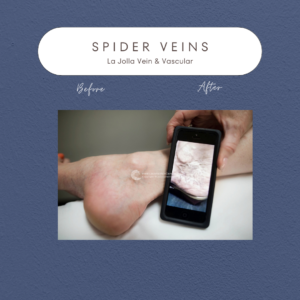
Real Transformations: Patient Success Stories
The journey to healthier veins is marked by visible transformations, as evidenced by the experiences of our patients who received vein treatment. These before-and-after images showcase the positive impact of effective treatment on individuals dealing with spider veins. The journey from discomfort and aesthetic concern to improved quality of life is a testimony to the importance of seeking the right care.
Spider veins might seem like a minor concern, but they can often be a window into underlying vascular issues. Understanding their causes, symptoms, and potential implications empowers individuals to seek appropriate solutions for their vein health. Whether it’s recognizing the significance of feeder veins, identifying signs of venous insufficiency, or acknowledging the various triggers behind spider veins, education is key. By choosing to address spider veins early on, individuals can embark on a path towards healthier, more comfortable lives.


“Bringing Experts Together for Unparalleled Vein and Vascular Care”
La Jolla Vein & Vascular (formerly La Jolla Vein Care) is committed to bringing experts together for unparalleled vein and vascular care.
Nisha Bunke, MD, Sarah Lucas, MD, and Amanda Steinberger, MD are specialists who combine their experience and expertise to offer world-class vascular care.
Our accredited center is also a nationally known teaching site and center of excellence.
For more information on treatments and to book a consultation, please give our office a call at 858-550-0330.
For a deeper dive into vein and vascular care, please check out our Youtube Channel at this link, and our website https://ljvascular.com
For more information on varicose veins and eliminating underlying venous insufficiency,
Please follow our social media Instagram Profile and Tik Tok Profile for more fun videos and educational information.
For more blogs and educational content, please check out our clinic’s blog posts!