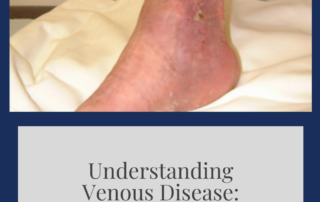
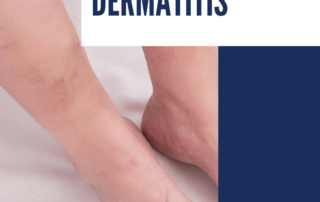
Causes of Non-Healing Ulcers & Wounds
Non-healing ulcers & wounds do not follow the usual healing process and are referred to as chronic wounds should they persist beyond 3 weeks. Such wounds can be a heavy burden to live with for anyone. Still, the board-certified vascular surgeons and specialists at La Jolla Vein & Vascular are dedicated to administering […]