Demystifying Venous Disease: Causes, Symptoms, and Treatment Options
Demystifying Venous Disease: Causes, Symptoms, and Treatment Options for Lasting Relief
Venous reflux disease, also known as venous insufficiency or venous stasis, is a complex condition that impacts the veins in the legs, affecting blood flow and circulation. Understanding the causes, recognizing the symptoms, and knowing the treatment options can help you manage this condition effectively. In this article, we’ll explore venous reflux disease from every angle—its root causes, how it progresses, and how ultrasound technology can guide personalized treatment plans for long-term relief.
Understanding Venous Reflux Disease
At the core of venous reflux disease is a malfunction in the valves within the veins of the legs. Normally, these valves work to keep blood flowing in the right direction, pushing it toward the heart. However, when these valves fail or become “leaky,” blood flows backward—a condition known as reflux—leading to the pooling of blood in the legs. This can affect both the deep and superficial veins, creating widespread inefficiencies in circulation.
The Anatomy of Venous Reflux
To better understand venous reflux, it’s essential to know the anatomy of the leg veins. The veins are broadly categorized into two types: deep veins and superficial veins.
- Deep Veins: Located within the muscles, deep veins carry the bulk of the blood from the legs back to the heart. They are critical for maintaining circulation.
- Superficial Veins: Positioned just under the skin, these veins are less involved in carrying large amounts of blood but can still be affected by venous reflux. Among them, the Great Saphenous Vein (GSV), which runs along the thigh and calf, and the Small Saphenous Vein (SSV), located along the back of the calf, play key roles.
Venous reflux in any of these veins can lead to significant discomfort and more severe complications over time.
Impact of Leaky Valves on Health
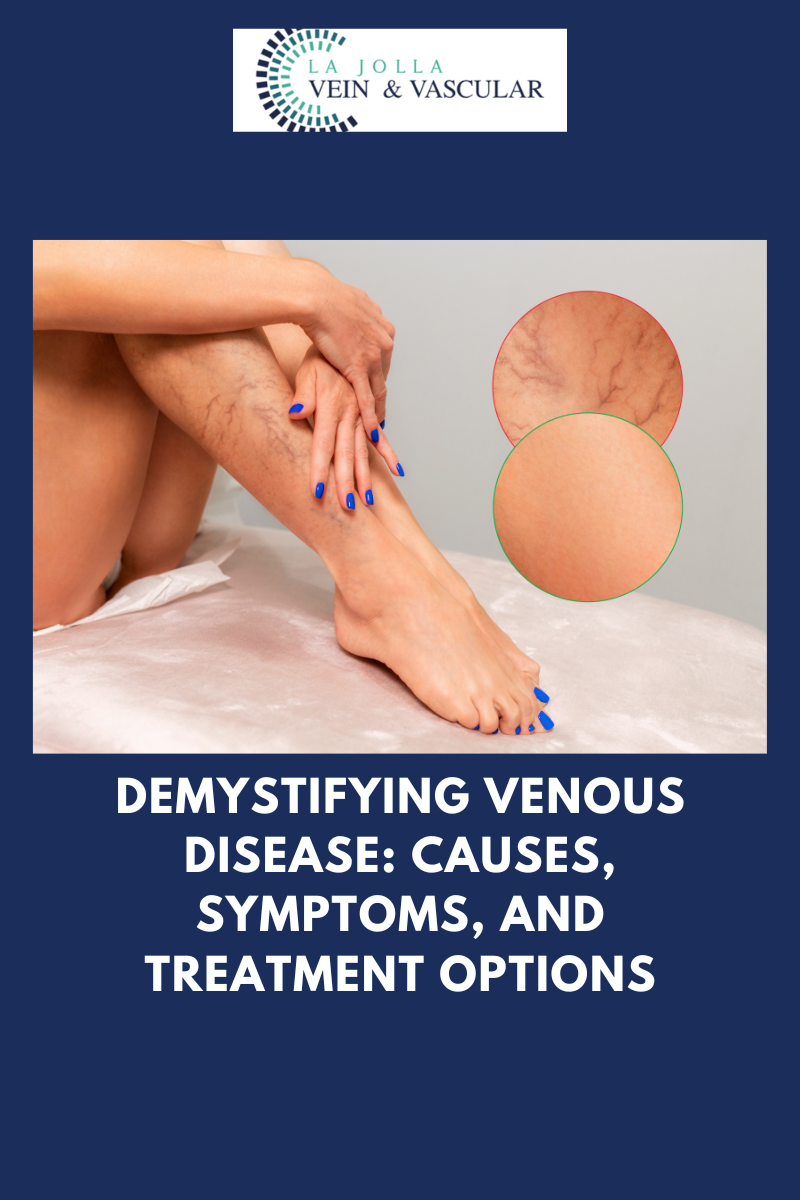
When the one-way valves in the leg veins malfunction, gravity causes blood to flow backward and pool in the lower legs. This process leads to several noticeable symptoms, including:
- Leg heaviness: A constant feeling of weight in the legs.
- Pain and fatigue: Persistent discomfort, particularly after long periods of standing.
- Swelling in the ankles: Blood pooling causes the ankles to swell, especially later in the day.
- Restless legs syndrome: Some people experience discomfort that worsens at night.
Over time, if left untreated, venous reflux disease may advance, resulting in skin changes such as:
- Darkening or discoloration around the ankles.
- Dry, itchy skin that may become irritated.
- Venous leg ulcers, which are open sores that can be difficult to heal.
These symptoms highlight the importance of early diagnosis and intervention to prevent disease progression.
The Role of Ultrasound in Diagnosis
Venous reflux is often invisible to the naked eye, especially when it involves deeper veins. As a result, a thorough diagnosis depends on ultrasound technology. This non-invasive tool helps physicians assess several critical aspects of vein function:
- The direction of blood flow to detect reflux.
- The condition of the valves to see if they are functioning properly.
- The presence of any blockages or scarring that could be exacerbating the condition.
By offering a detailed view of the veins beneath the skin, ultrasound serves as an invaluable resource for formulating targeted treatment plans.
Personalized Treatment Options for Venous Reflux Disease
Treating venous reflux disease requires a patient-centered approach. Every case is unique, and treatment plans must be tailored to the specific needs and conditions of the patient. Here’s an overview of the general steps involved in treating venous reflux disease:
Step 1: Treating the Underlying Reflux
The first priority is to address the root cause of the issue—venous reflux in the saphenous veins. Several innovative procedures are available to correct this problem, including:
- Radiofrequency Ablation: This method uses heat to close off the leaky veins.
- Laser Ablation: Like radiofrequency, this technique employs laser energy to seal the affected veins.
- Mechanico-Chemical Ablation (MOCA): A combination of mechanical disruption and chemical agents to treat the reflux.
- Varithena Foam: A foamed solution injected into the vein, which causes it to close and reroutes blood to healthier veins.
By addressing reflux at its source, these treatments restore proper blood flow and prevent further complications.
Step 2: Eliminating Varicose Veins
After treating the underlying reflux, attention shifts to removing the visible, bulging veins. Varicose veins are often treated through:
- Foam sclerotherapy: A procedure that involves injecting a foamed medication into the vein to collapse it.
- Minimally invasive vein removal: Techniques like ambulatory phlebectomy, where the varicose veins are gently extracted through small punctures in the skin.
These methods offer effective relief from both the symptoms and the appearance of varicose veins.
Step 3: Cosmetic Treatment for Spider Veins
For patients interested in improving the cosmetic appearance of their legs, spider vein treatment is the final step. These small, superficial veins can be treated with sclerotherapy, which involves injecting a solution to close the veins, improving the overall look of the skin. While spider veins are not typically a health concern, this treatment is a popular option for enhancing aesthetic appeal.
Venous Reflux Disease: A Comprehensive Approach to Care
Venous reflux disease is a condition that impacts not only your health but also your quality of life. Fortunately, with modern diagnostic tools like ultrasound and advanced treatment options such as vein ablation, varicose vein removal, and sclerotherapy, it is possible to manage this condition effectively. At La Jolla Vein & Vascular, we are dedicated to delivering personalized, cutting-edge care that addresses every aspect of venous reflux disease, from diagnosis to treatment. Our goal is to restore your vascular health and help you live more comfortably.
If you’re ready to begin your journey toward healthier veins, contact us today to schedule a consultation. Our team of experienced specialists is here to guide you every step of the way.