The Best Way to Treat Reticular Veins
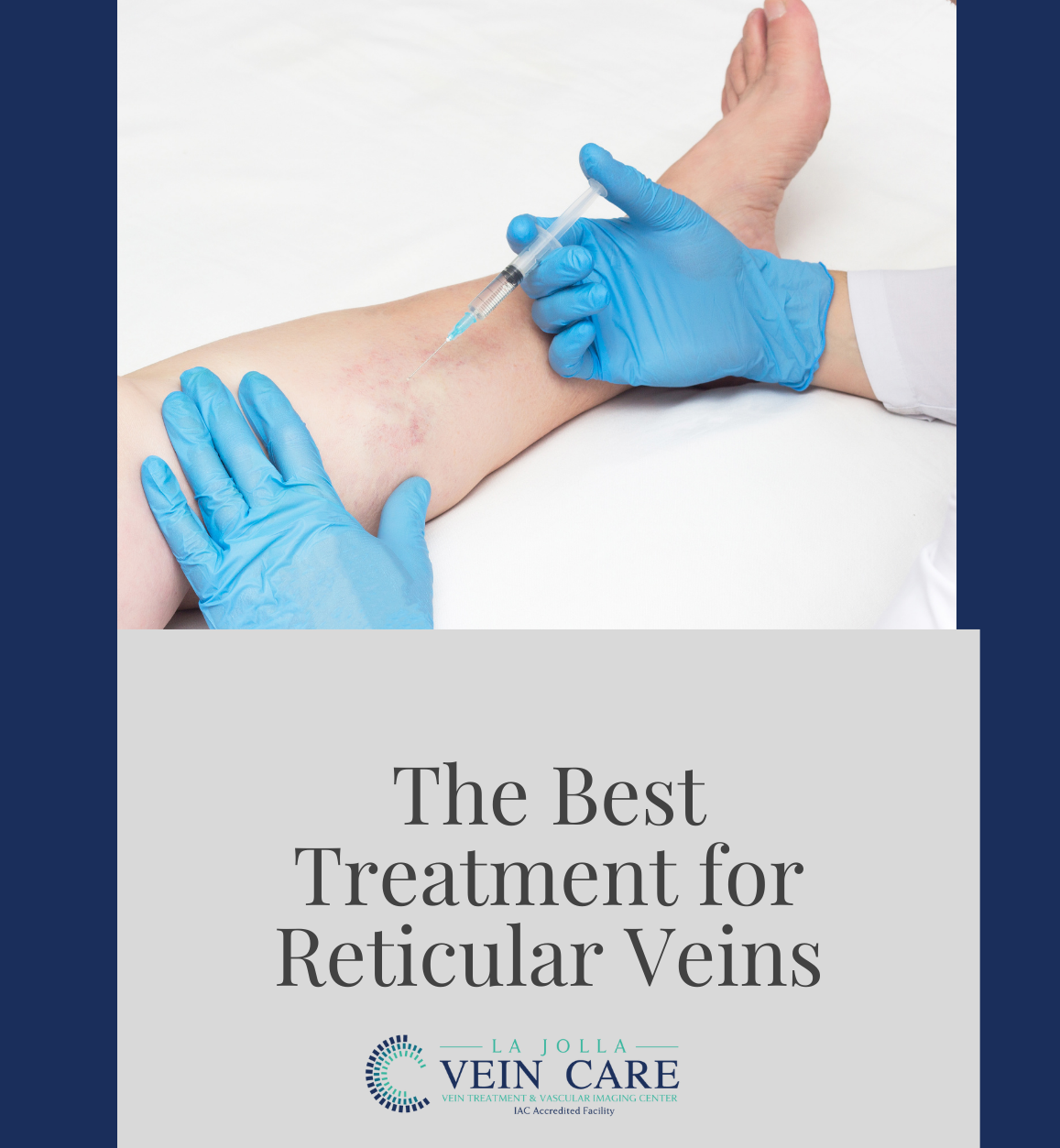
LJVascular2025-10-15T22:41:54-07:00The best treatment for Reticular Veins is through a painless alternative to traditional sclerotherapy: Cryo-Sclerotherapy.
Why have I been offered cryo-sclerotherapy?
We recommend patients undergo cry-sclerotherapy to mainly treat spider veins and small varicose veins at the skin surface (also known as reticular veins). Traditional sclerotherapy involves injection of a medication into the […]