Treatment for reticular veins
LJVascular2022-10-24T11:12:10-07:00The best treatment for Reticular Veins is through a painless alternative to traditional sclerotherapy: Cryo-Sclerotherapy.
Why have I been offered cryo-sclerotherapy?
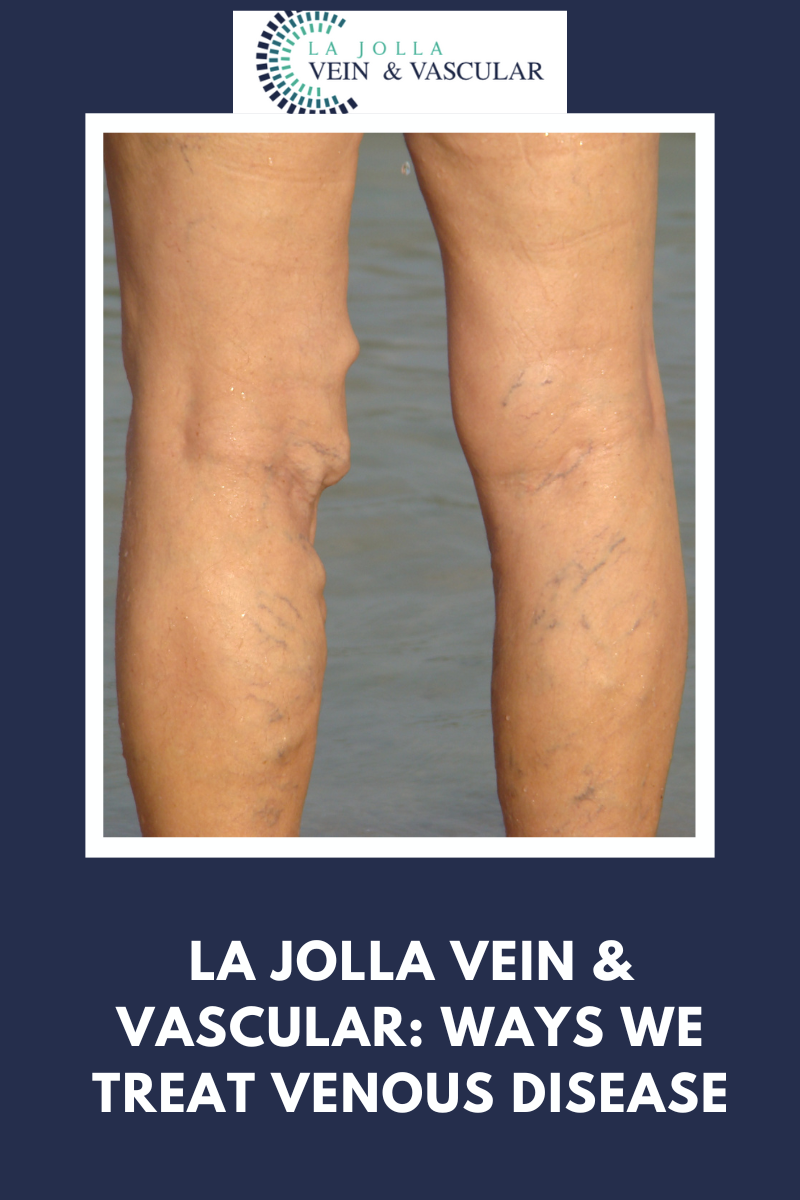
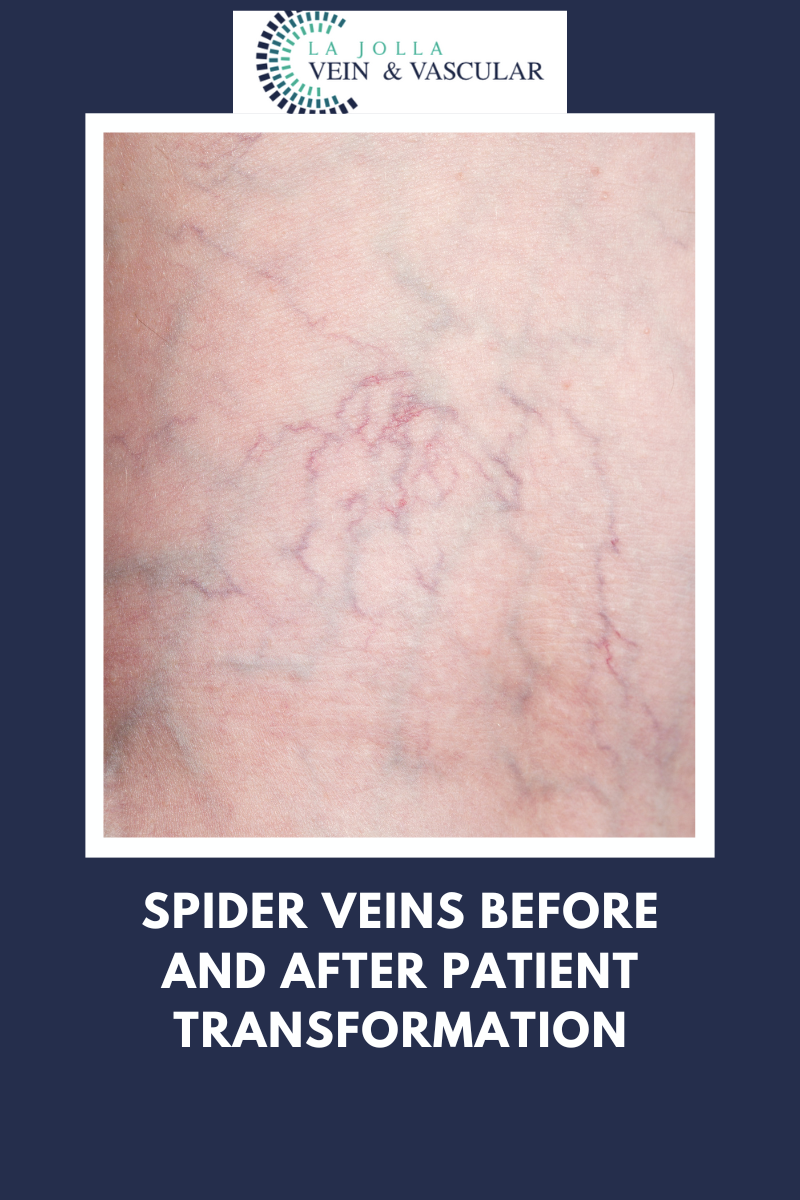
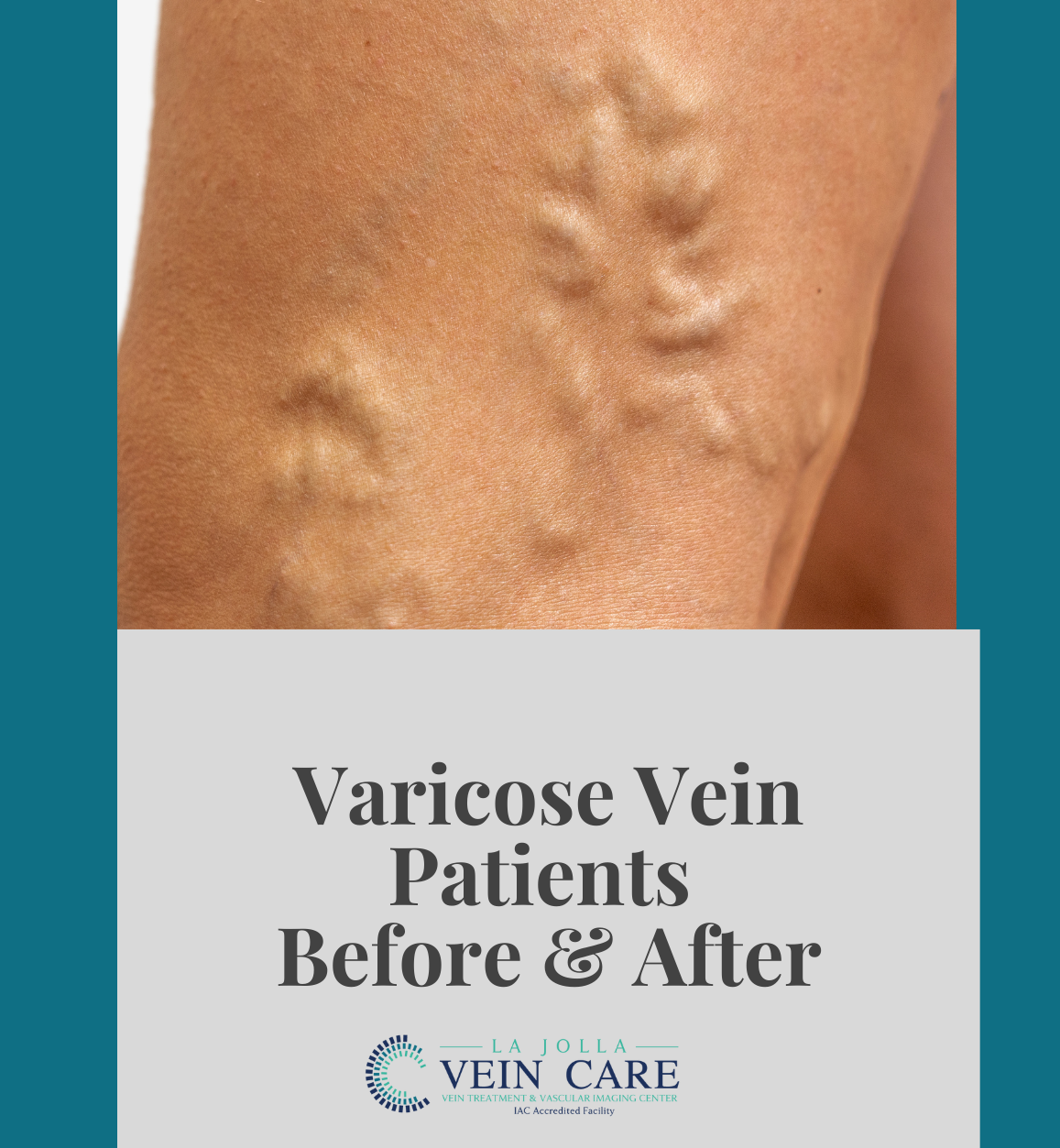
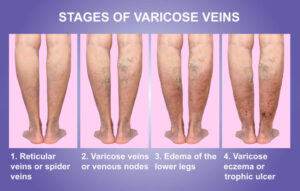
We recommend patients undergo cry-sclerotherapy to mainly treat spider veins and small varicose veins at the skin surface (also known as reticular veins). Traditional sclerotherapy involves injection of a medication into the vein using a tiny needle. This causes the vein to collapse and eventually fade away. The medication will be administered in a liquid and /or foam formulation, depending on the size of the veins. Cryo-sclerotherapy is the combination of traditional sclerotherapy in combination with the use of a cryo device. The cryo device delivers puffs of cold air simultaneously during sclerotherapy. The result is the cold air anesthetizes the skin so the treatment is relatively painless. This is especially helpful for treatment of sensitive areas like the inner ankles and thighs. Instead of feeling the needle prick, you will feel puffs of cold air instead. The cold air may also reduce bruising and pain.
What should I expect on my treatment days?
You will sign your consent form then change into shorts provided by the office. We will clean your skin with alcohol. The sclerosant medication will then be injected into your veins with a fine needle. Just before the needle is used, you will feel puffs of cold air. The cold air will anesthetize the skin, so that the prick from the needle is not felt or lessened. Every time the needle is used, you will feel puffs of cold air instead. After your treatment, we will help you into your compression stockings, then you will walk for 30 minutes prior to getting in your car. It is normal for your legs to be achy and tender to the touch after treatment.
What should I do after treatment?
You will be instructed on how long to wear compression stockings after treatment, depending on the size of the veins that are treated. Most patients wear thigh-high compression stockings continuously for 1-3 days, then another 7 days.
You may shower with the stockings on or take a quick cool shower with them off.
You should walk 30 minutes twice daily after treatment and move your legs frequently throughout the day with short walks and/or calf exercises. This avoids pooling of blood in the legs. Avoid prolonged sitting during the day.
It is normal to have aching in the treated veins. This responds well to walking, ice packs, and anti-inflammatory medications such as ibuprofen (Advil, Motrin) and naproxen (Aleve).
What should I avoid after treatment?
For at least two weeks after treatment, you should avoid strenuous exercise (anything more than a brisk walk), heavy lifting, saunas or hot tubs, and leg massages. All of these dilate the superficial veins and interfere with their healing. You should also avoid airline travel for two weeks after treatment.
What are the possible side effects?
You will likely have some bruising over the injection sites, then the treated veins may become firm and blue.
The skin overlying treated veins may also develop brownish hyperpigmentation as the blood products within those veins are absorbed by the body; in some patients it can take up to a year to fade. Some patients temporarily develop some very fine, pink spider veins in areas where veins have been treated (telangiectatic matting). These usually resolve spontaneously over several weeks but occasionally require additional treatment to clear.
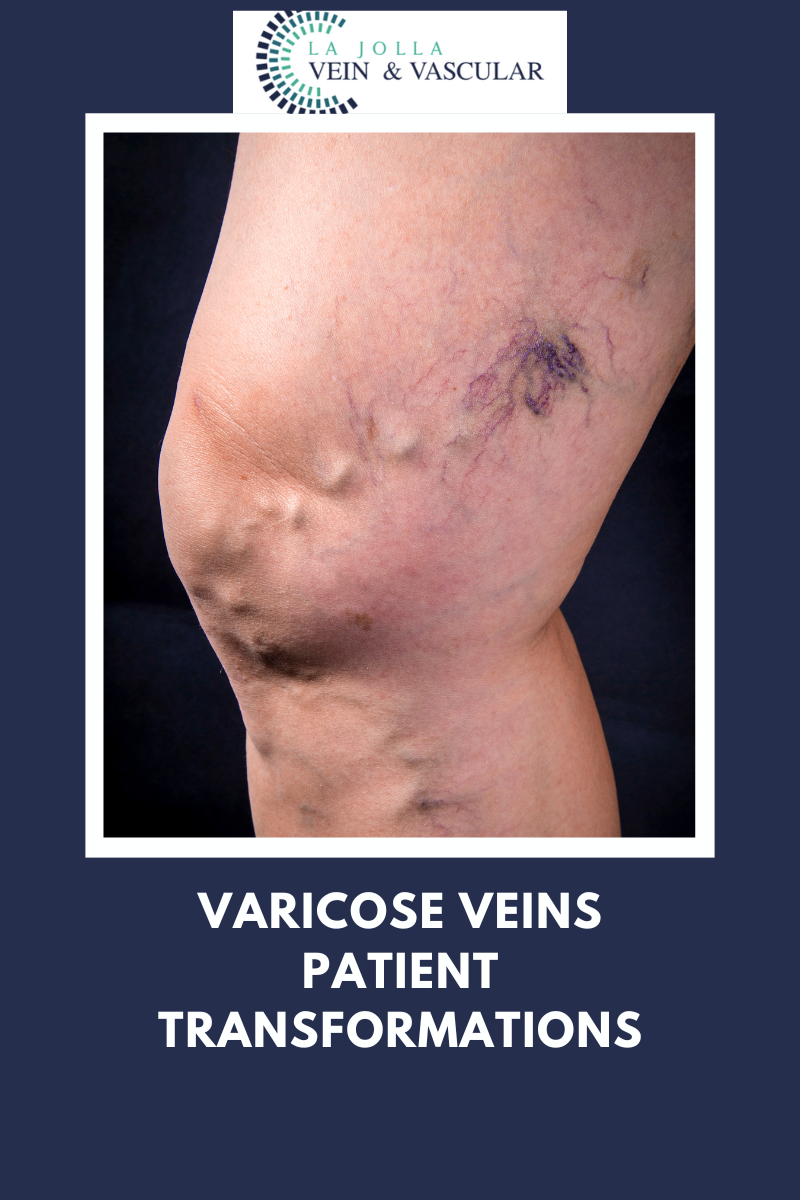
Many patients will feel their veins look a bit worse in the first month after sclerotherapy, but through the best treatment for reticular veins, cryo-sclerotherapy, patients have reported it to be a more painless approach for treatment.
La Jolla Vein & Vascular (formerly La Jolla Vein Care) is committed to bringing experts together for unparalleled vein and vascular care.
Nisha Bunke, MD, Sarah Lucas, MD, and Elliot DeYoung, MD are specialists who combine their experience and expertise to offer world-class vascular care.
Our accredited center is also a nationally known teaching site and center of excellence.
For more information on treatments and to book a consultation, please give our office a call at 858-550-0330.
For a deeper dive into vein and vascular care, please check out our Youtube Channel at this link.
For more information on varicose veins and eliminating underlying venous insufficiency, check this link out full of resources.