Signs of Venous Disease
LJVascular2022-07-20T15:06:13-07:00Signs of Chronic Venous Insufficiency & Venous Disease
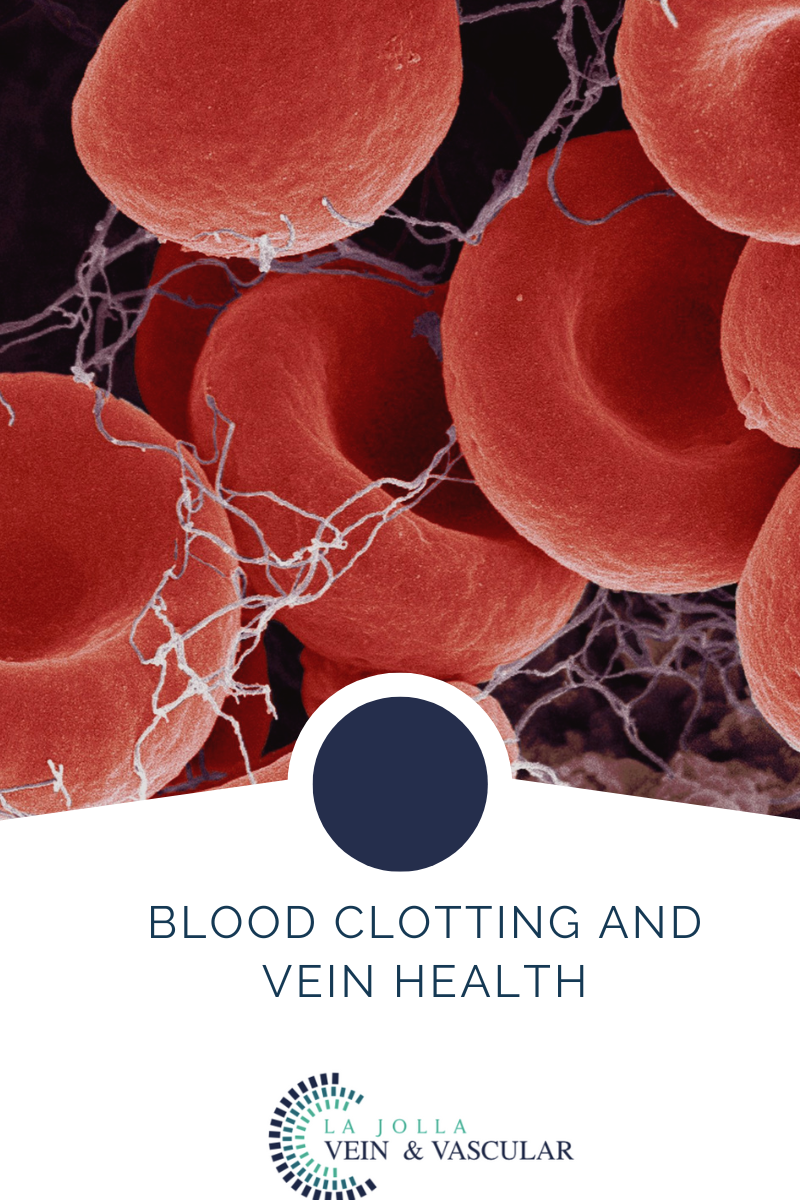
Chronic venous insufficiency (CVI) is an inflammatory condition caused by long standing, untreated venous reflux disease which can cause very unique signs and symptoms. Commonly, venous reflux disease causes a collection of symptoms such as leg swelling, heaviness, fatigue and varicose veins. But, over […]