Cosmetic Sclerotherapy
LJVascular2023-01-14T13:33:03-08:00Sclerotherapy Treatment for Spider Veins
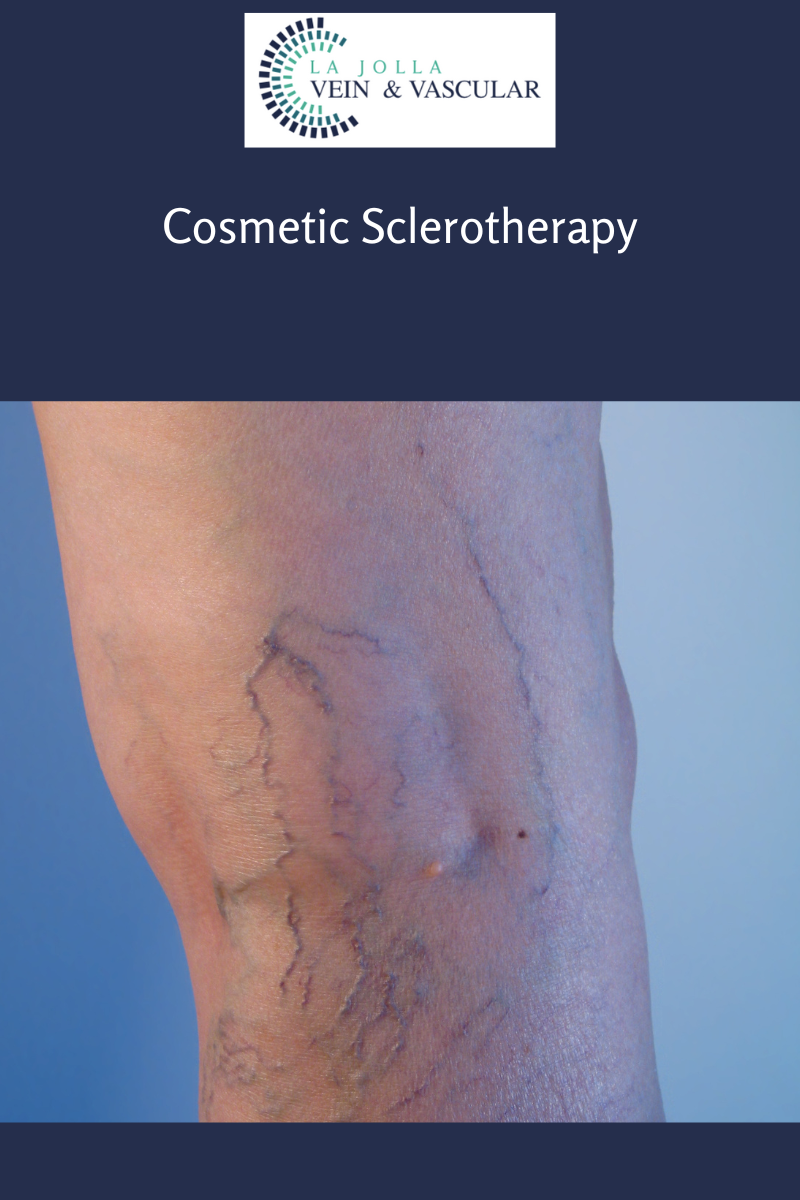
You have been recommended to have sclerotherapy injections. Spider veins and reticular veins of the legs are most commonly treated with sclerotherapy. Sclerotherapy involves an injection of a medication into the vein. This will cause the vein to collapse and gradually fade away. Sclerotherapy has been used to treat spider veins for decades, but newer solutions such as AscleraTM allow for spider veins to be treated with minimal discomfort and immediate return to activities. Vein specialists rarely use saline solutions these days, because alternative solutions are less painful and better tolerated. Sclerotherapy is preferred by most vein specialists over laser because spider veins often have underlying ‘feeder veins’ that can easily be treated with sclerotherapy, but are not addressed by laser. Many people will require more than one treatment session for optimal results. The national average is 2 to 5 treatment sessions. Treatment sessions are often spaced a month apart, but your health care provider will help determine your customized care plan. Wearing compression stockings after treatment will improve results.
For larger veins, the medication may be turned into a foam, this is referred to as foam sclerotherapy. Foam sclerotherapy is similar to sclerotherapy of spider veins but instead of a liquid solution, a foamed-solution is injected directly into the vein via a small needle. The solution can be seen on ultrasound monitoring which allows it to be directed into nearby varicose veins painlessly. The veins will seal shut, and gradually be broken down by the body.
“Bringing Experts Together for Unparalleled Vein and Vascular Care”
La Jolla Vein & Vascular (formerly La Jolla Vein Care) is committed to bringing experts together for unparalleled vein and vascular care.
Nisha Bunke, MD, Sarah Lucas, MD, and Elliot DeYoung, MD are specialists who combine their experience and expertise to offer world-class vascular care.
Our accredited center is also a nationally known teaching site and center of excellence.
For more information on treatments and to book a consultation, please give our office a call at 858-550-0330.
For a deeper dive into vein and vascular care, please check out our Youtube Channel at this link.
For more information on varicose veins and eliminating underlying venous insufficiency, check this link out full of resources.
Please follow our social media Instagram Profile and Tik Tok Profile for more fun videos and educational information.