The Best Way to Treat Spider Veins
LJVascular2022-03-17T10:12:50-07:00The best way to treat spider veins is through a procedure called Sclerotherapy. At La Jolla Vein Care we have seen great patient transformations with this type of therapy. If you are interested in knowing if you have spider veins, check this article out.
Sclerotherapy
Why was I recommended to have sclerotherapy injections?
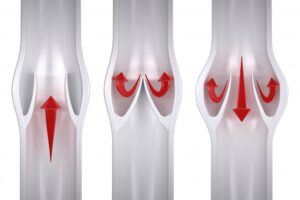
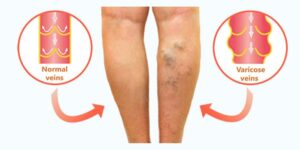
Spider veins and reticular veins of the legs are most commonly treated with sclerotherapy. Sclerotherapy involves an injection of a medication into the vein. This will cause the vein to collapse and gradually fade away. Sclerotherapy has been used to treat spider veins for decades, but newer solutions such as Asclera allow for spider veins to be treated with minimal discomfort and immediate return to activities.
Vein specialists rarely use saline solutions these days, because alternative solutions are less painful and better tolerated. Sclerotherapy is preferred by most vein specialists over laser because spider veins often have underlying feeder veins that can easily be treated with sclerotherapy, but are not addressed by laser. Many people will require more than one treatment session for optimal results. The national average is 2 to 5 treatment sessions. Treatment sessions are often spaced a month apart, but your health care provider will help determine your customized care plan. Wearing compression stockings after treatment will improve results.
For larger veins, the medication may be turned into a foam, this is referred to as foam sclerotherapy. Foam sclerotherapy is similar to sclerotherapy of spider veins but instead of a liquid solution, a foamed-solution is injected directly into the vein via a small needle. The solution can be seen on ultrasound monitoring which allows it to be directed into nearby varicose veins painlessly. The veins will seal shut, and gradually be broken down by the body.
What should I expect on my treatment days?
You will sign your consent form then change into shorts provided by the office. We will clean your skin with alcohol. The sclerosant medication will then be injected into your veins with a fine needle. After your treatment, we will help you into your compression stockings, then you will walk for 30 minutes prior to getting into your car. It is normal for your legs to be achy and tender to the touch after treatment.
What should I do after treatment?
You will be instructed on how long to wear compression stockings after treatment, depending on the size of the veins that are treated. Most patients wear thigh-high compression stockings continuously for 1-3 days, then another 7 days. You may shower with the stockings on or take a quick cool shower with them off.
You should walk 30 minutes twice daily after treatment and move your legs frequently throughout the day with short walks and/or calf exercises. This avoids pooling of blood in the legs. Avoid prolonged sitting during the day.
It is normal to have aching in the treated veins. This responds well to walking, ice packs, and anti-inflammatory medications such as ibuprofen (Advil, Motrin) and naproxen (Aleve).
What should I avoid after treatment?
For at least two weeks after treatment, you should avoid strenuous exercise (anything more than a brisk walk), heavy lifting, saunas or hot tubs, and leg massages. All of these dilate the superficial veins and interfere with their healing. You should also avoid airline travel for two weeks after treatment.
What are the possible side effects?
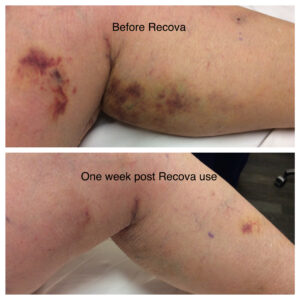
You will likely have some bruising over the injection sites, then the treated veins may become firm and blue.
The skin overlying treated veins may also develop brownish hyperpigmentation as the blood products within those veins are absorbed by the body; in some patients it can take up to a year to fade. Some patients temporarily develop some very fine, pink spider veins in areas where veins have been treated (telangiectatic matting). These usually resolve spontaneously over several weeks but occasionally require additional treatment to clear. If you notice the spider veins have not gone away after treatment, this information may be helpful for you.
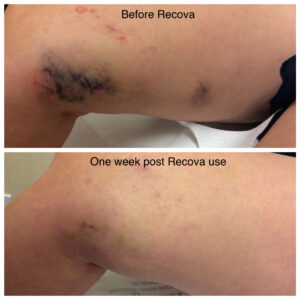
Below are the before and after transformations that we have seen in patient cases with spider veins and sclerotherapy.