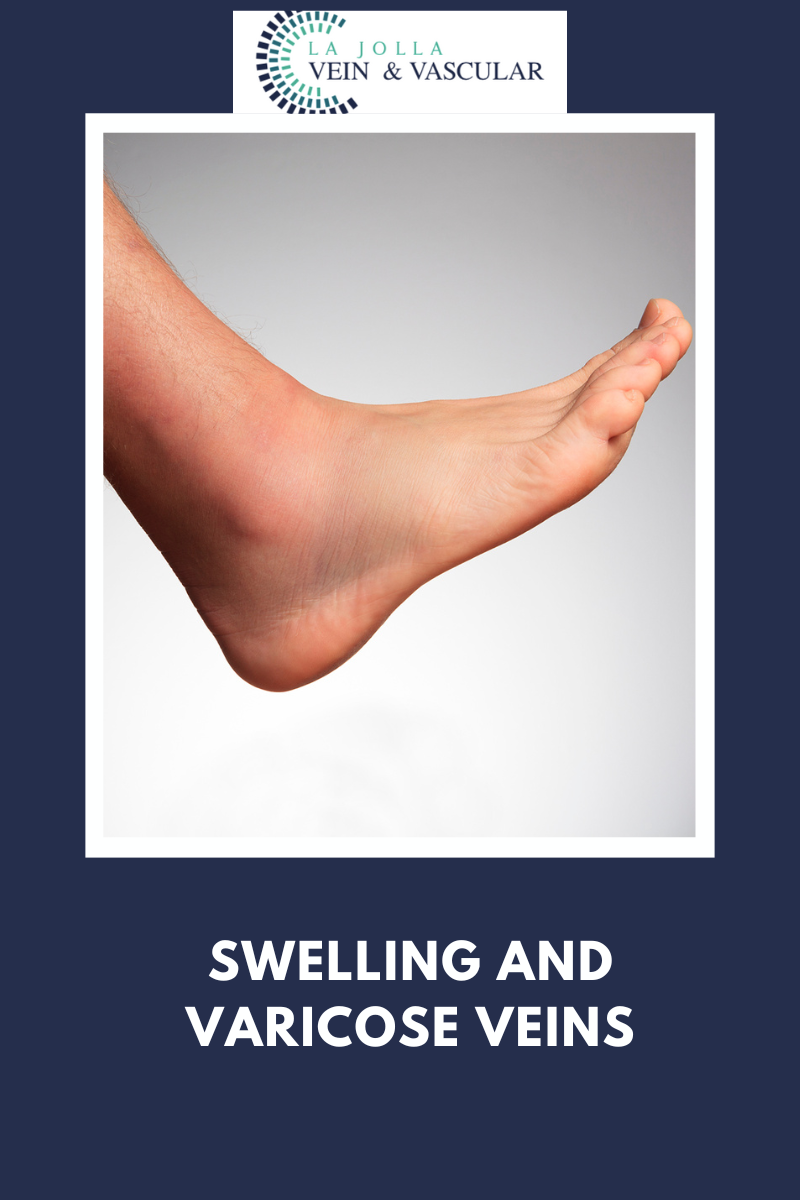
Swelling & Varicose Veins
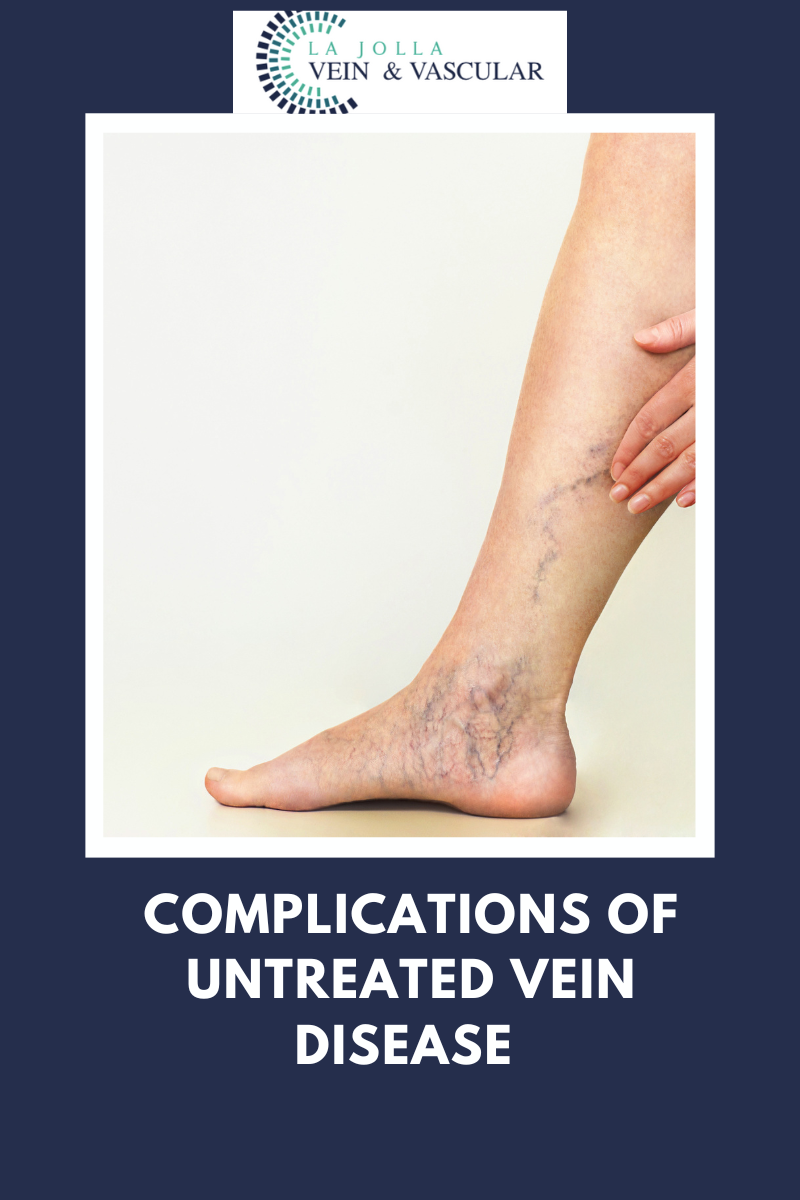
LJVascular2022-07-19T17:52:04-07:00Complications of Untreated Varicose Veins and Venous Insufficiency: Swelling of the Ankles/legs
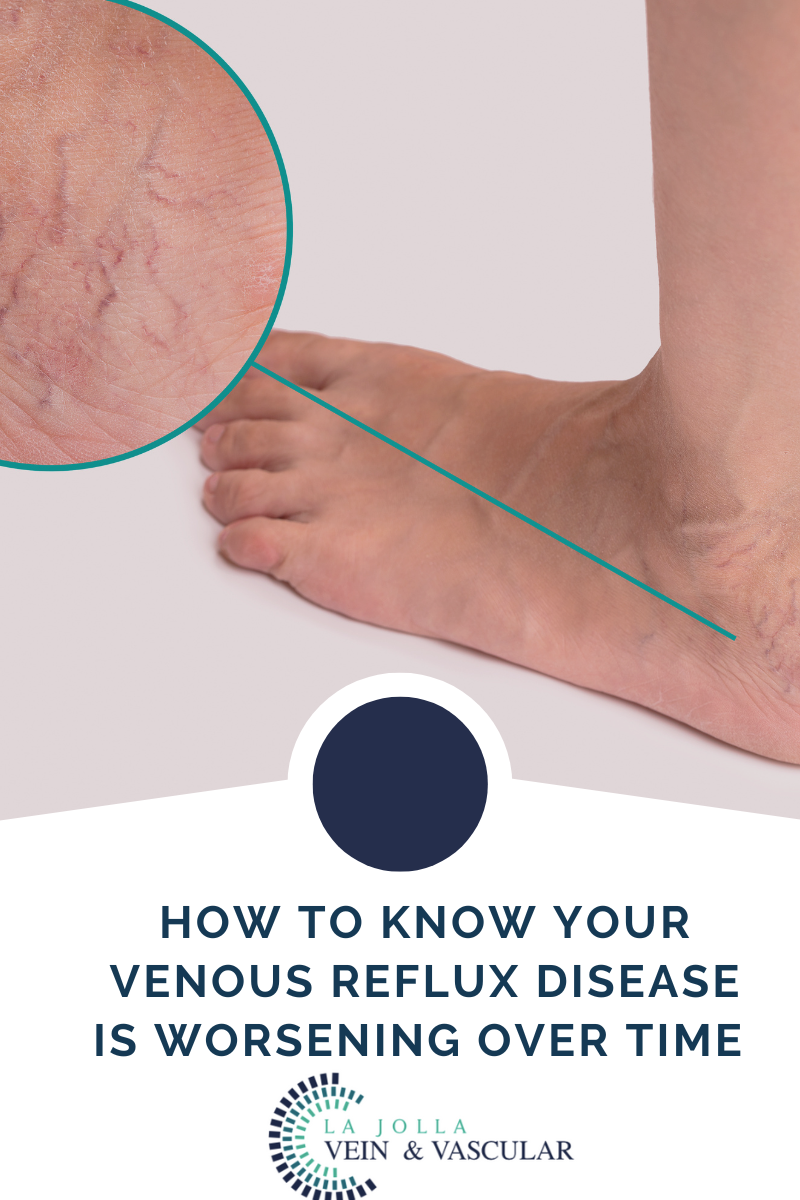
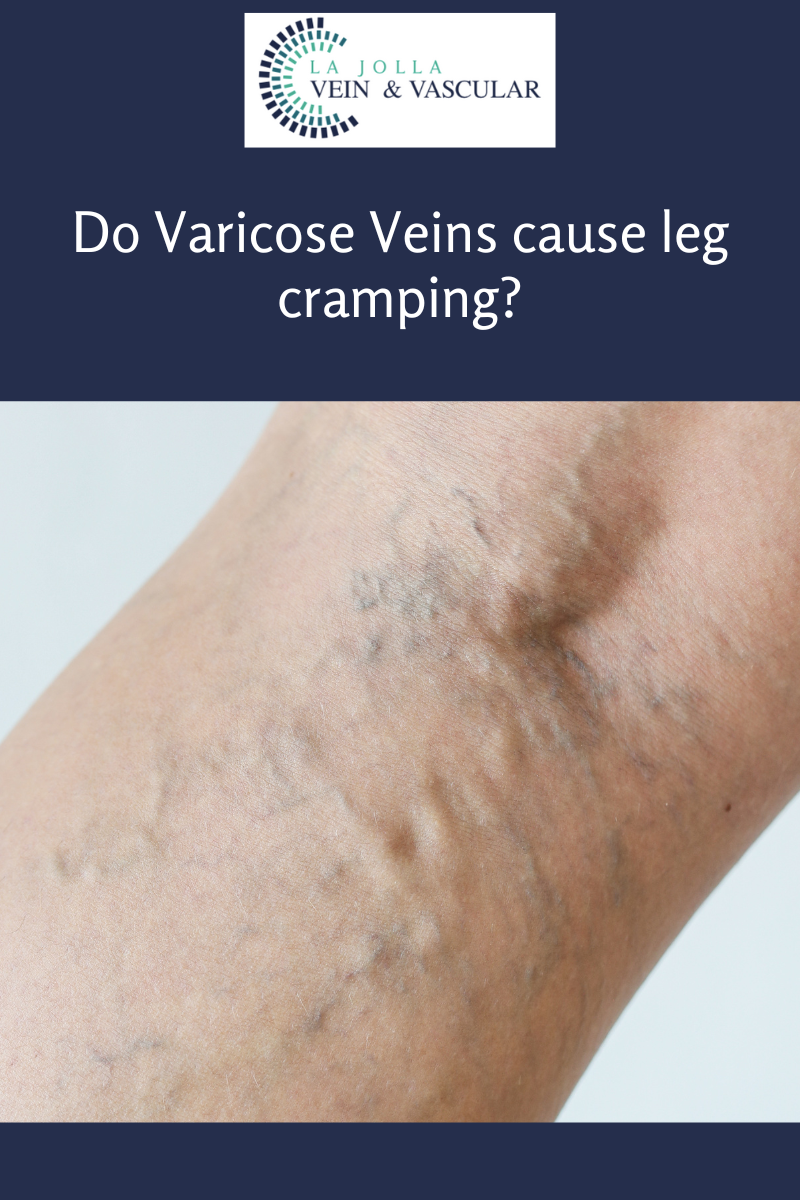
Leg swelling (swelling is also known as edema), is a common complaint related to varicose veins and underlying venous insufficiency. Leg swelling can be present simply from underlying venous insufficiency without visible signs of varicose veins or spider veins. As […]